EFIC COVID-19 Task Force
The EFIC COVID-19 Task Force was created after realizing the need for news related to COVID-19 being distributed and shared with our community which is looking for advice with regards to pain treatment of their patients. The intended outcome is to distribute relevant news on our website and other communication channels. Our goal here is to put forward what is being said in an objective manner and provide a neutral overview on current research. The information will of course be updated as more research becomes available.
Task Force Members
Roger Knaggs, University of Nottingham, United Kingdom
Felicia Cox, Royal Brompton and Harefield Hospitals, United Kingdom
Martin Galligan, The Royal Marsden School, United Kingdom
Edmund Keogh, University of Bath, United Kingdom
Mary O’Keeffe, European Pain Federation EFIC, Belgium
Gisèle Pickering, University Hospital Estaing of Clermont-Ferrand, France
Michael Schäfer, Charité Universitätsmedizin, Germany
Reviews & Opinion
Effects of COVID-19 on cognition and brain health (Cell Press. November 2023).
Read the full article here.
Post-COVID Pain Syndromes (Current Pain and Headache Reports (2022))
Read the full article here.
Does aspirin save lives in patients with COVID-19? (Heart. 2022 Jan)
Read the full article here.
Further evidence for the use of aspirin in COVID-19 (Int J Cardiol . 2022 Jan)
Read the full article here.
What lies behind and beyond acute COVID- 19 pain?
Read the full article here.
Timing of musculoskeletal steroid injections in pain practice during Coronavirus disease 2019 (COVID-19) vaccine administration
Read the full article here.
Steroid injections in pain management: influence on coronavirus disease 2019 vaccines
Read the full article here.
COVID-19 and chronic fatigue syndrome: An endocrine perspective
Read the full article here.
Headache as an acute and post-COVID-19 symptom in COVID-19 survivors: A meta-analysis of the current literature (Eur J Neurol. 2021 Nov)
Read the full article here.
Practical recommendations for the management of the patient with chronic pain during the pandemic of COVID-19 (Rev Esp Anestesiol Reanim (Engl Ed). 2021 Nov)
Read the full article here.
Headache as a Symptom of COVID-19: Narrative Review of 1-Year Research (Curr Pain Headache Rep. 2021 Nov)
Read the full article here.
Emergency department care for patients who use opioids during the COVID-19 pandemic (CJEM . 2021 Nov)
Read the full article here.
Use of steroids in COVID-19 patients: A meta-analysis (Epub. 2021)
Read the full article here.
Telehealth Increases Access to Brief Behavioral Interventions in Orofacial Pain Clinic during COVID-19 Pandemic: A Retrospective Study (Pain Med. 2021 Oct)
Read the full article here.
Mental and neurological disorders and risk of COVID-19 susceptibility, illness severity and mortality: A systematic review, meta-analysis and call for action (EClinicalMedicine . 2021 Oct)
Read the full article here.
Insight into pain syndromes in acute phase of mild-to-moderate COVID-19: Frequency, clinical characteristics, and associated factors
Read the full article here.
Perioperative use of intra-articular steroids during the COVID-19 pandemic. (Eur J Orthop Surg Traumatol. 2021 Sep)
Read the full article here.
COVID-19, Suffering and Palliative Care: A Review. (Am J Hosp Palliat Care. 2021 Sep)
Read the full article here.
Physical and mental health complications post-COVID-19: Scoping review ( J Psychosom Res. 2021 Aug)
Read the full article here.
COVID-Pain: Acute and Late-Onset Painful Clinical Manifestations in COVID-19 - Molecular Mechanisms and Research Perspectives ( J Pain Res. 2021 Aug)
Read the full article here.
Commentary: Management of Intractable Pain in Patients With Implanted Spinal Cord Stimulation Devices During the COVID-19 Pandemic Using a Remote and Wireless Programming System ( Front Neurosci. 2021 Aug)
Read the full article here.
Interventions for palliative symptom control in COVID-19 patients ( Cochrane Database Syst Rev. 2021 Aug)
Read the full article here.
Pain Management in Children During the COVID-19 Pandemic (Curr Anesthesiol Rep. 2021 Jul )
Read the full article here.
Headache as an acute and post-COVID-19 symptom in COVID-19 survivors: A meta-analysis of the current literature (Eur J Neurol. 2021 Jul)
Read the full article here.
COVID-19 Among Patients With Multiple Sclerosis A Systematic Review (2021 July)
Read the full article here.
Pain during and after coronavirus disease 2019: Chinese perspectives (2021)
Read the full article here.
Biological, psychological, and social factors associated withworsening of chronic pain during the first wave of the COVID-19pandemic: a cross-sectional survey (2021)
Read the full article here.
Practical Advices for Treating Chronic Pain in the Time of COVID-19: A Narrative Review Focusing on Interventional Techniques (J Clin Med. 2021 Jun)
Read the full article here.
Review article on COVID-19 and Guillain-Barré syndrome ( Front Biosci (Schol Ed) . 2021 Jun)
Read the full article here.
Upsurges in the joblessness and opioid epidemics in the United States after the COVID-19 epidemic: the plight of the jobless patient in the clinic (Pain. 2021 June)
Read the full article here.
Pain Management for Dental Medicine in 2021: Opioids, Coronavirus and Beyond. (Pain Res 2021)
Read the full article here.
Non-steroidal anti-inflammatory drug use and outcomes of COVID-19 in the ISARIC Clinical Characterisation Protocol UK cohort: a matched, prospective cohort study (May 2021)
Read the full article here.
Postdischarge rheumatic and musculoskeletal symptoms following hospitalization for COVID-19: prospective follow-up by phone interviews (May 2021)
Read the full article here.
Nonsteroidal Antiinflammatory Drugs and Susceptibility to COVID-19 ( Arthritis Rheumatol 2021 May)
Read the full article here.
The impact of Coronavirus disease 2019 (COVID‐19) pandemic on migraine disorder (J Neurol. 2021 May )
Read the full article here.
Chronic Pain Management during the Covid-19 Pandemic: A Scoping Review (April 2021)
Read the full article here.
Download PDFPDF Download PDF + Supplemental DataPDF + Supplementary Material Commentary Inadequate reporting of COVID-19 clinical studies: a renewed rationale for the Sex and Gender Equity in Research (SAGER) guidelines (April 2021)
Read the full article here.
Headache related to mask use of healthcare workers in COVID-19 pandemic ( Korean J Pain Apr 2021)
Read the full article here.
Why COVID-19 strengthens the case to scale up assault on non-communicable diseases: role of health professionals including physical therapists in mitigating pandemic waves (Apr 2021)
Read the full article here.
Migraine during COVID-19: Data from Second Wave Pandemic in an Italian Cohort. (Brain Sciences Apr 2021)
Read the full article here.
Migraine treatment and COVID-19 vaccines: No cause for concern (Headache. 2021 Mar)
Read the full article here.
The psychiatric and neuropsychiatric repercussions associated with severe infections of COVID-19 and other coronaviruses (Mar 2021)
Read the full article here.
Pain management and prevention of suicide in the COVID-19 era (Eur Arch Psychiatry Clin Neurosci. 2021 Mar)
Read the full article here.
Effects of the COVID-19 pandemic on chronic pain in Spain: a scoping review. (Pain Rep. 2021 Feb.)
Read the full article here.
The Social Forces Healing Patients with Painful Conditions: What Happens After COVID-19? (Pain Med. 2021 Feb.)
Read the full article here.
The neurological symptoms of COVID-19: a systematic overview of systematic reviews, comparison with other neurological conditions and implications for healthcare services. (Ther Adv Chronic Dis. 2021 Jan)
Read the full article here.
Pain Symptoms in Patients with Coronavirus Disease (COVID-19): A Literature Review. (J Pain Res. 2021 Jan.)
Read the full article here.
Pain during and after COVID-19 in Germany and worldwide: a narrative review of current knowledge. (Pain Rep. 2021 Jan.)
Read the full article here.
Pain Management During the COVID-19 Pandemic (Pain Ther. 2020 Dec)
Read the full article here.
Collateral Damage as Crises Collide: Perioperative Opioids in the COVID-19 Era. (Pain Med. 2020 Nov.)
Read the full article here.
The social threats of COVID-19 for people with chronic pain. (Pain. 2020 Oct.)
Read the full article here.
Rheumatic manifestations of COVID-19: a systematic review and meta-analysis. (BMC Rheumatol. 2020 Oct.)
Read the full article here.
Managing patients with rheumatic diseases during the COVID-19 pandemic: The French Society of Rheumatology answers to most frequently asked questions up to May 2020. (Joint Bone Spine. 2020 Oct.)
Read the full text here.
Daring discourse: are we ready to recommend neuraxial anesthesia and peripheral nerve blocks during the COVID-19 pandemic? A pro-con. (Reg Anesth Pain Med. 2020 Oct.)
Read the full article here.
COVID-19 and Headache Medicine: A Narrative Review of Non-Steroidal Anti-Inflammatory Drug (NSAID) and Corticosteroid Use. (Headache. 2020 Sep.)
Read the full article here.
Medications in COVID-19 patients: summarizing the current literature from an orthopaedic perspective. (Int. Orthop. 2020 Aug.)
Read the full article here.
Gastrointestinal involvement in COVID-19: a systematic review and meta-analysis. (Ann Gastroenterol. 2020 Jul-Aug.)
Read the full article here.
Safety of ibuprofen in patients with COVID-19: causal or confounded? (CHEST. 2020 Jul.)
Type of article: Commentary
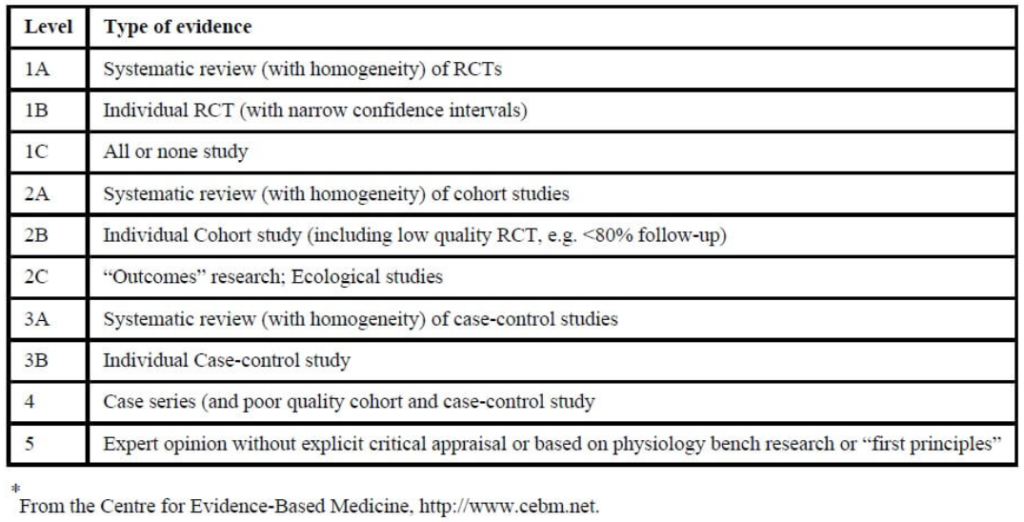
Level of evidence: 5 (Expert opinion without explicit critical appraisal or based on physiology bench research or first principles)
Results: This commentary retraces the origins of the worldwide alarm towards the use of ibuprofen, starting with a tweet from the French Health Minister who, after 4 young people reportedly developed serious COVID-19 disease after taking NSAIDs, advised that ibuprofen could aggravate the infection. The report, although unpublished, was reported in The BMJ and endorsed by specialists from France and UK, and by the WHO.
The authors criticise the low level of evidence of these reports, as well as the notion, published in The Lancet, that ibuprofen could enhance coronavirus infectivity by increasing the bioavailability of angiotensin converter enzyme (ACE), to which the virus binds. They argue that drawing conclusions from theoretical pharmacology is dangerous and can lead to erroneous results, such as the hypothesis that co-administration of ibuprofen and aspirin could counteract antiplatelet effectiveness, which was based on pharmacological thromboxane levels but then refuted in a randomized controlled trial.
Implications: Rather than concluding that ibuprofen is safe for COVID-19 related fever, the authors observe that current epidemiologic evidence “is not strong enough to infer a causal link of a harmful effect of ibuprofen in COVID-19”. They advise, however, that patients with COVID-19 take acetaminophen monotherapy for fever reduction.
Commentary: A very interesting critique of the multiple biases and insufficiencies that have polluted medical literature on this topic. It is, however, amusing that after such a clear analysis the authors end up recommending the same approach –paracetamol (acetaminophen) – as the French Minister in his initial tweet.
Reviewed by EFIC on April 23, 2020 – read the article in full here.
Pain: A Potential New Label of COVID-19 (Brain, Behavior, Immunity. 2020 Jul.)
Type of study: Letter to editor
Level of evidence: 5 (Expert opinion without critical opinion or based on physiology bench research or first principles)
Results: Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has been identified as the pathogen of COVID-19. The spike protein on this virus binds the angiotensin-converting enzyme 2 (ACE2) receptor, mediating entry into human cells. Studies have also detected SARS-CoV-2 in the cerebrospinal fluid of infected patients. Although the expression of ACE2 receptor in the human nervous system has not been fully identified, ACE2 has been detected in neurons and microglia in the spinal dorsal horn of mice.
The study suggests that SARS-CoV-2 might infect ACE2-positive cells in human spinal dorsal horn and decrease functional ACE2 activity resulting in the accumulation of angiotensin-II and decrease of angiotensin (1-7). Consequently, SARS-CoV-2 infection in the spinal cord may induce pain.
Implications: The potential burden of pain induced by COVID-19 cannot be ignored. However, the role of the ACE2 receptor in pain transmission and pain management for people infected with SARS-CoV-2 needs further scientific and clinical studies, in order to guide treatment and public health policy.
Commentary: There is no definitive evidence yet on the importance of this mechanism in humans, but a scientifically sound hypothesis is proposed. Yet, we should be cautious when drawing conclusions from mechanistic or theoretical pharmacology, especially from rodents, as a number of examples show that such evidence can later be refuted by clinical data.
Reviewed by EFIC on May 15, 2020 – read the full article here
Does Ibuprofen Worsen COVID-19? (Drug Safety. 2020 Jun.)
Moore N, Carleton B, Blin P, Bosco-Levy P, Droz C. Drug Saf. 2020 Jul;43(7):611-614. doi: 10.1007/s40264-020-00953-0. No abstract available.PMID: 32529474 [PubMed – indexed for MEDLINE] Free PMC Article
Read the full article here
Grappling with Chronic Pain and Poverty during the COVID-19 Pandemic (June 2020)
Read the full article here
Neurological and Musculoskeletal Features of COVID-19: A Systematic Review and Meta-Analysis. (Front. Neurol. 2020 Jun.)
Read the full article here.
Involvement of digestive system in COVID-19: manifestations, pathology, management and challenges. (Therap. Adv. Gastroenterol. 2020 Jun.)
Read the full article here.
No current evidence supporting risk of using Ibuprofen in patients with COVID‐19. (Int. J. Clin. Pract. 2020 Jun.)
Read the full article here.
Management of osteoarthritis during COVID-19 pandemic (Clinical Pharmacology and Therapeutics. 2020 May.)
Type of study: Review
Level of evidence: 3A (less systematic review of a variety of study designs, including in-vitro, in-vivo, animal and human-studies.)
Population: People with osteoarthritis
Results: NSAIDs: No evidence for discontinuation
Corticosteroids: No evidence for discontinuation of systemic treatment
Opioids: No evidence for discontinuation – the authors recommend weak opioids with no immunosuppressive activity
Monoclonal Antibodies (mAbs): No evidence for experimental use of mAbs in OA and COVID-19 patients except compassionate use or within clinical trials
Commentary: This paper does not add new findings to the existing literature but offers a good one-stop review for the specific care of patients with osteoarthritis. Overall, therapies for osteoarthritis appear to be safe and there is not any clear indication to avoid prescription or suggest discontinuation of existing pharmacological therapies due to COVID-19 infection or its complications.
The authors preference for weak opioids without immunosuppressive activity is subjective opinion and may be dose-related. High dose weak opioid may have similar effects as low dose strong opioids. Although different opioids vary in their effects on the immune system, any clinical relevance is still uncertain.
The authors acknowledge that decisions need to be scrutinized in the high inflammatory stage of COVID-19 infection.
Reviewed by EFIC on May 20, 2020 – Read the full article here
COVID-19 is a Real Headache! (Headache Journal. 2020 May.)
Type of study: Views and perspectives
Level of evidence: 2A (systematic review of cohort studies)
Results: Initial reported symptoms of SARS‐CoV‐2 infection were mainly respiratory, and were characterised by fever, sore throat, cough, and dyspnoea. Other symptoms, including headache, abdominal pain, diarrhoea, loss of taste and smell, have been added as possible symptoms of COVID-19 over time. Reports of neurological symptoms are increasing rapidly, and headache appears to be most common. Headache has been reported in 11%-34% of hospitalized COVID-19 patients, however clinical features of these headaches are not reported. The authors experience suggest significant features of headache presentation in symptomatic COVID-19 patients were new-onset, moderate-severe, bilateral headache with pulsating or pressing quality in the temporoparietal, forehead or periorbital region. The most striking features of the headache were variable onset and poor response to common analgesics, or high relapse rate, that was limited to the active phase of the COVID-19.
Implications: As a common non-respiratory symptom of COVID-19, headache should not be overlooked, and its characteristics should be recorded with scrutiny. If headache is ignored as a symptom of COVID-19, there may be delay in diagnosis, leading to further infection cases in the community.
Commentary: Clinical features of headache related have to COVID-19 have not been well documented. A case vignette is described and several possible pathophysiological mechanisms are proposed from theoretical considerations.
Reviewed by EFIC on May 20, 2020 – Read the full article here
Model based approach for estimating the dosage regimen of indomethacin a potential antiviral treatment of patients infected with SARS CoV-2 (Journal of Pharmacokinetics and Pharmacodynamics. 2020 May.)
Type of study: Mini-review and theoretical model of optimal dosage
Population: in vitro studies; in vivo animal studies
Results: Indometacin, an anti-inflammatory drug, has been used as symptomatic treatment to improve oxygenation in patients with acute respiratory distress [Hanly et al Lancet 1987; Steinberg et al Circ Shock 1990] and to reduce proinflammatory interleukin-6 levels [Sacerdote et al Inflamm Res 1995]. In addition, indometacin has been shown to have potent in-vitro antiviral properties against human SARS-CoV-1, canine CCoV, and more recently on human SARS CoV-2 [Amici et al Antivir Ther. 2006, Xu et al Front Med J. 2020].
In this paper the authors propose indometacin as a promising candidate for the treatment of SARS-CoV-2 and try to provide criteria for comparing benefits of alternative dosage regimens using a model-based approach. They characterize % of recovery and viral load in CCoV-infected dogs, to estimate the PK of indometacin in dog and human using published data after administration of immediate (IR) and sustained-release (SR) formulations, and to estimate the expected antiviral activity as a function of different assumptions on the effective exposure in human.
Implications: Should indometacin prove active against SARS CoV-2 in humans, the best theoretical dosing regimens modelled were 50 mg three-times-a-day for the IR formulation, and 75 mg twice-a-day for the SR formulation.
Commentary: The main interest of this paper is in the reference list, which provides published data on the efficacy of Indometacin on various coronaviruses including COVID-1 and COVID-2, in vitro, in dogs, and potentially in humans. Should current clinical trial using indometacin (that started April 2020) be positive, this study provides a PK/PD basis to determine best therapeutic regimens. Of particular note, indomethacin has a higher toxicity index than other NSAIDs, including ibuprofen (especially GI related) and the recommended dosing is relatively high. So, a gastroprotective drug should be indicated also.
Reviewed by EFIC on May 28, 2020 – read the full article here
A Review. Neuropathogenesis and Neurologic Manifestations of the Coronaviruses in the Age of Coronavirus Disease 2019. (JAMA Neurol. 2020 May.)
Read the full article here.
Identifying rheumatic disease patients at high risk and requiring shielding during the COVID-19 pandemic. (Clin. Med. (Lond). 2020 May.)
Read the full article here.
Headache medication and the COVID-19 pandemic (Journal of Headache Pain, 2020 Apr.)
Type of article: Commentary, brief literature analysis
Level of evidence: 5 (Expert opinion without explicit critical appraisal or based on physiology bench research or first principles)
Population: Patients suffering chronic headache and treated with ACE inhibitors (ACE-I), angiotensin II receptor blockers (ARB) or ibuprofen
Results: Concern has arisen in view of a putative link between the use of inhibitors of the renin-angiotensin system (ACE-I, ARB) and ibuprofen and an increased risk for COVID-19 infection. The authors discuss this concern in relation to headache treatment and conclude that, based on current evidence, there is no reason to abandon treatment with ACEI, ARB or ibuprofen in people with headache. There is no convincing evidence in medical / research literature that either renin-angiotensin system blockers or ibuprofen worsen SARS-CoV-2 infection in any type of patient, including headache patients.
Implications: The authors, in agreement with the advice of international cardiovascular societies, see no rationale to alter the prescription of these drugs that have an important role in the treatment of headache.
Commentary: There is no reason, empirical or scientific, to discontinue a treatment with ACE-I/ARB or ibuprofen in patients with COVID-19 infection. Discussion on mechanisms is short but sensible and rich. Conclusions are in line with recent results from Zhang et al (Circ. Res 2020, doi: 10.1161/CIRCRESAHA.120.317134.), that shows absence of complications and even better outcome in hypertensive patients with Covid19 treated with ACE-I/ARB.
Reviewed by EFIC on May 15, 2020 – read the full article here.
Associations between immune-suppressive and stimulating drugs and novel COVID-19 (eCancer. 2020 Mar.)
Type of study: Review
Level of evidence: 3A (systematic review of a variety of study types including in-vitro-, case-, in-vivo, animal- and human studies).
Results: NSAIDs: The search did not identify any strong evidence for or against the use of ibuprofen for treatment of COVID-19 specifically.
Corticosteroids: Some evidence that corticosteroids may be beneficial in the treatment of SARS-CoV. However, this is not specific to COVID-19.
Commentary: There is no definitive evidence that NSAIDs or corticosteroids are contraindicated in COVID-19.
Reviewed by EFIC on April 23, 2020 – read the full article here.
Cannabidiol as prophylaxis for SARS-CoV-2 and COVID-19? Unfounded claims versus potential risks of medications during the pandemic (RSAP. 2020 Mar.)
Type of study: Letter to the Editor
Level of evidence: 5 (Expert opinion without explicit critical appraisal or based on physiology bench research or first principles)
Results: During the COVID-19 pandemic, many patients may look for natural remedies to protect themselves. Use of products containing cannabinoids have proliferated amidst claims of health benefits including immune “support” or “boosting”. Cannabidiol (CBD) and tetrahydrocannabinol (THC) have complex pharmacological properties, including anti-inflammatory effects, that may be useful in certain conditions (including autoimmune and neurodegeneration diseases). However, they suppress cytokines, chemokines, effector T-cells, and microglial cells, reducing the host response to pathogens including viruses like SARS-CoV-2.
Implications: Current pharmacological and clinical evidence suggest CBD and THC decrease the body’s ability to fight infections, in particular viral and respiratory infections. In a clinical trial of cannabidiol for epilepsy, respiratory infections (pneumonia) were over 30% more common in those receiving CBD versus placebo. The author recommends avoiding the use of cannabinoids during this pandemic unless medically supported for recognised indications (e.g. seizures, cancer, chronic pain), and highlights false marketing claims of medical benefit including “immune system boosting” or antiviral effects, that should be reported to regulatory bodies.
Commentary: A very concise yet well-documented summary of the potentially serious problems of health-marketing as applied to cannabis. The analysis is USA-centred, where the direct advertisement and marketing of medicines is greater than in Europe.
Reviewed by EFIC on April 23, 2020 – read the full article here.
How psychosocial and economic impacts of COVID-19 pandemic can interfere on bruxism and temporomandibular disorders? (J. Appl. Oral. Sci. 2020.)
Read the full article here.
Population Studies & Case Studies
Worsening pain and quality of life for spine surgery patients during the COVID-19 pandemic: Roles of psychological distress and patient activation (N Am Spine Soc J. 2022 Mar)
Read the full article here.
Depressive Symptoms Associated With Musculoskeletal Pain in Inactive Adults During COVID-19 Quarantine (Pain Manag Nurs. 2022 Feb)
Read the full article here.
Corticosteroids for COVID-19 symptoms and quality of life at 1 year from admission (J Med Virol. 2022 Jan)
Read the full article here.
Long COVID: rheumatologic/musculoskeletal symptoms in hospitalized COVID-19 survivors at 3 and 6 months (Clin Rheumatol. 2022 Jan)
Read the full article here.
The profile of musculoskeletal pain and its associations with sleep quality and depression during the COVID-19 in Turkey (Korean J Pain. 2022 Jan)
Read the full article here.
Neurological complications after first dose of COVID-19 vaccines and SARS-CoV-2 infection (Nat Med. 2021 Dec)
Read the full article here.
Characteristics and influence on quality of life of new-onset pain in critical COVID-19 survivors (Eur J Pain. 2021)
Read the full article here.
Characteristics and Risk Factors of Persistent Neuropathic Pain in Recovered COVID-19 Patients (Pain Med. 2021 Dec)
Read the full article here.
GP consultation rates for sequelae after acute covid-19 in patients managed in the community or hospital in the UK: population based study (BMJ. 2021Dec)
Read the full article here.
Acute worsening of clinical presentation in CRPS after SARS-CoV-2 (COVID-19) vaccination: a case series (Pain Management. 2022 Nov)
Read the full article here.
Post-COVID-19 longitudinally extensive transverse myelitis: is it a new entity? (Neurol Sci. 2021 Nov)
Read the full article here.
Effects of COVID-19 Social Distancing Measures in Individuals with Chronic Pain Living in Spain in the Late Stages of the Lockdown (Int J Environ Res Public Health. 2021 Nov)
Read the full article here.
COVID-19 outcomes among adult patients treated with long-term opioid therapy for chronic non-cancer pain in the USA: a retrospective cohort study (BMJ Open. 2021 Nov)
Read the full article here.
Do Anxiety and Depression Predict Persistent Physical Symptoms After a Severe COVID-19 Episode? A Prospective Study (Front. Psychiatry. November 2021)
Read the full article here.
The impact of the COVID-19 pandemic on people with rheumatic and musculoskeletal diseases: insights from patient-generated data on social media (Rheumatology (Oxford). 2021 Oct)
Read the full article here.
Decrease in pain perception during acute severe acute respiratory syndrome coronavirus 2 infection: a case series (Pain. 2021 Oct)
Read the full article here.
Intravenous lidocaine infusion in a case of severe COVID-19 infection (J Anaesthesiol Clin Pharmacol. 2021 Jul-Sep)
Read the full article here.
Specialist palliative and end-of-life care for patients with cancer and SARS-CoV-2 infection: a European perspective. (Ther Adv Med Oncol. 2021 Sep)
Read the full article here.
Pain experience and social support of endometriosis patients during the COVID-19 pandemic in Germany - results of a web-based cross-sectional survey. (PLoS One. 2021 Aug)
Read the full article here.
The Impact of the First Wave of the COVID-19 Pandemic on Patients' Perceptions of Chronic Pain. (J Pain Res. 2021 Aug)
Read the full article here.
One Year of COVID-19 Pandemic in Italy: Effect of Sedentary Behavior on Physical Activity Levels and Musculoskeletal Pain among University Students. (Int J Environ Res Public Health. 2021 Aug)
Read the full article here.
The impact of COVID-19 on opioid use in those awaiting hip and knee arthroplasty : A retrospective cohort study. (BMJ Qual Saf. 2021 Aug)
Read the full article here.
Musculoskeletal symptoms and related factors in postacute COVID-19 patients ( Int J Clin Pract. Aug 2021)
Read the full article here.
Toward a better understanding of persistent headache after mild COVID-19: Three migraine-like yet distinct scenarios ( Headache. Aug 2021)
Read the full article here.
Gastrointestinal symptoms and healthcare utilization have increased among patients with functional gastrointestinal and motility disorders during the COVID-19 pandemic ( Neurogastroenterol Motil. Aug 2021)
Read the full article here.
Extended Neuralgic Amyotrophy Syndrome in a Confirmed COVID-19 Patient After Intensive Care Unit and Inpatient Rehabilitation Stay. (Am J Phys Med Rehab. Aug 2021)
Read the full article here.
Guillain-Barré Syndrome Variant Occurring after SARS-CoV-2 Vaccination ( Ann Neurol. Aug 2021)
Read the full article here.
Coronavirus disease-19 and headache; impact on pre-existing and characteristics of de novo: a cross-sectional study. (J Headache and Pain. Aug 2021)
Read the full article here.
Post-COVID-19 exacerbation of fibrodysplasia ossificans progressiva with multiple flare-ups and extensive heterotopic ossification in a 45-year-old female patient (Rheumatol Int . 2021 Aug)
Read the full article here.
Effect of COVID-19 on management of patients with low back pain in the emergency department ( Australas Emerg Care. Jul 2021)
Read the full article here.
Understanding Experiences of Fibromyalgia Patients Involved in the Fimouv Study During COVID-19 Lockdown (Front. Psychol. Jul 2021)
Read the full article here.
Headache Attributed to Vaccination Against COVID-19 with the ChAdOx1 nCoV-19 (AZD1222) Vaccine: A Multicenter Observational Cohort Study. (Pain Ther. Aug 2021)
Read the full article here.
New daily persistent headache after SARS-CoV-2 infection: a report of two cases. (Neurol Sci. Jul 2021)
Read the full article here.
Back Pain Prevalence, Intensity, and Associated Risk Factors among Female Teachers in Slovakia during the COVID-19 Pandemic: A Cross-Sectional Study (Healthc. Jul 2021)
Read the full article here.
Factors associated with COVID-19-related death in people with rheumatic diseases: results from the COVID-19 Global Rheumatology Alliance physician-reported registry (Ann Rheum Dis. 2021 Jul)
Read the full article here.
Non-steroidal anti-inflammatory drug use and outcomes of COVID-19 in the ISARIC Clinical Characterisation Protocol UK cohort: a matched, prospective cohort study (2021, July)
Read the full article here.
Psychological impact of COVID-19 pandemic on TMD subjects ( Eur Rev Med Pharmacol Sci . 2021 Jul)
Read the full article here.
Frequency and phenotype of headache in covid-19: a study of 2194 patients ( Sci Rep. 2021 Jul)
Read the full article here.
Impact of COVID-19 on the pain and disability of patients with adult spinal deformity ( Spine Deform. 2021 Jul)
Read the full article here.
Neuropathic pain post-COVID-19: a case report ( BMJ Case Rep. 2021 Jul)
Read the full article here.
Clinical manifestations and outcome of SARS-CoV-2 infections in children and adolescents with rheumatic musculoskeletal diseases: data from the National Paediatric Rheumatology Database in Germany ( RMD Open. 2021 Jul)
Read the full article here.
Effects of the COVID-19 lockdown on musculoskeletal pain, physical activity, and work environment in Estonian office workers transitioning to working from home (Work. 2021)
Read the full article here.
Back pain: An aftermath of Covid-19 pandemic? A Malta perspective (Musculoskelet Care. 2021)
Read the full article here.
Impact of COVID-19 pandemic social restriction measures on people with rheumatic and musculoskeletal diseases in the UK: a mixed-methods study (BMJ 2021)
Read the full article here.
Postdischarge rheumatic and musculoskeletal symptoms following hospitalization for COVID-19: prospective follow-up by phone interviews ( Rheumatol Int . 2021)
Read the full article here.
Prevalence and characteristics of new-onset pain in COVID-19 survivours, a controlled study. (Eur J Pain July 2021)
Read the full article here.
Physical and mental impact of COVID-19 outbreak on fibromyalgia patients. (Clin Exp Rheumatol. May-Jun 2021)
Read the full article here.
Primary headaches during the COVID-19 lockdown in Germany: analysis of data from 2325 patients using an electronic headache diary ( J. Headache Pain. 2021, June)
Read the full article here.
The effects of COVID-19 fear and anxiety on symptom severity, sleep quality, and mood in patients with fibromyalgia: a pilot study ( Adv Rheumatol. 2021 Jun)
Read the full article here.
The presence of headache at onset in SARS-CoV-2 infection is associated with long-term post-COVID headache and fatigue: A case-control study (Cephalalgia. 2021 Jun)
Read the full article here.
COVID-19-Induced Left Sciatic Neuropathy Requiring Prolonged Physical Medicine and Rehabilitation (2021, June)
Read the full article here.
No evidence for an effect of working from home on neck pain and neck disability among Swiss office workers: Short-term impact of COVID-19 ( Eur Spine J . 2021 Jun)
Read the full article here.
Effect of lockdown during COVID-19 on migraine: A longitudinal cohort study (Cephalalgia 2020)
Read the full article here.
The impact of COVID-19 pandemic on headache symptoms and drug withdrawal among patients with medication overuse headache: a cross-sectional study (J Headache Pain. 2021)
Read the full article here.
The effect of the COVID-19 Pandemic on anxiety, depression, and musculoskeletal system complaints in healthcare workers (Work. May 2021)
Read the full article here.
Pain and Anxiety due to the COVID-19 Pandemic. A Survey of Patients with Delayed Elective Hip and Knee Arthroplasty (Arthroplast Today. 2021)
Read the full article here.
Gender differences in health anxiety and musculoskeletal symptoms during the COVID-19 pandemic ( J Back Musculoskelet Rehabil 2021)
Read the full article here.
Impact of the COVID-19 pandemic on the pharmacological, physical, and psychological treatments of pain: findings from the Chronic Pain & COVID-19 Pan-Canadian Study (Pain Rep 2021)
Read the full article here.
6-month neurological and psychiatric outcomes in 236 379 survivors of COVID-19: a retrospective cohort study using electronic health records (May 2021)
Read the full article here.
Anaesthesia-related drugs and SARS-CoV-2 infection (Brit J Anaesth. Apr 2021)
Read the full article here.
Pain Manifestations of COVID-19 and Their Association With Mortality: A Multicenter Prospective Observational Study (Mayo Clin Proc. Apr 2021)
Read the full article here.
Pain Symptoms in COVID-19 (Apr 2021)
Read the full article here.
COVID-19-related cancellation of elective orthopaedic surgery caused increased pain and psychosocial distress levels (Knee Surg Sports Traumatology Arthrosc. Mar 2021)
Read the full article here.
Impact of COVID-19 on utilization of nonpharmacological and pharmacological treatments for chronic low back pain and clinical outcomes (J Osteopath Med. 2021 Mar)
Read the full article here.
Trigeminal neuralgia as the sole neurological manifestation of COVID-19: A case report (Mar 2021)
Read the full article here.
Pain and function deteriorate in patients awaiting total joint arthroplasty that has been postponed due to the COVID-19 pandemic (Mar 2021)
Read the full article here.
The Psychological Functioning in the COVID-19 Pandemic and Its Association With Psychological Flexibility and Broader Functioning in People With Chronic Pain ( J Pain Mar 2021)
Read the full article here.
Acute impact of a national lockdown during the COVID-19 pandemic on wellbeing outcomes among individuals with chronic pain. (J. Health. Psychol. 2021 Feb.)
Read the full article here.
Evaluation of the Impact of the COVID-19 Lockdown in the Clinical Course of Migraine. (Feb 2021)
Read the full article here.
No Evidence for a Decrease in Physical Activity Among Swiss Office Workers During COVID-19: A Longitudinal Study. (Feb 2021)
Read the full article here.
Pain in Chronic Pancreatitis During the COVID-19 Lockdown: Has It Given Us a New Dimension for Treatment? (Cureus Feb 2021)
Read the full article here.
The Early Impact of COVID-19 on Chronic Pain: A Cross-Sectional Investigation of a Large Online Sample of Individuals with Chronic Pain in the United States, April to May, 2020. (Pain Med. 2021 Feb.)
Read the full article here.
Brachial Plexus Neuropathies During the COVID-19 Pandemic: A Retrospective Case Series of 15 Patients in Critical Care. (Phys Ther. 2021 Jan.)
Read the full article here.
Management of Intractable Pain in Patients With Implanted Spinal Cord Stimulation Devices During the COVID-19 Pandemic Using a Remote and Wireless Programming System (Front. Neurosci. 2020 December)
Read the full article here.
A possible increased risk of metamizole-associated neutropenia among COVID-19 patients. (Br. J. Clin. Pharmacol. 2020 Dec.)
Read the full article here.
Coronavirus disease 2019 (COVID-19) and ischemic colitis: An under-recognized complication (The American Journal of Emergency Medicine. 2020 Dec.)
Type of study: Case reports
Level of evidence: 4 (Case studies)
Population: Two people with COVID-19 presenting with abdominal pain
Results:
Case 1:
-
Male, 73 years old, hypertension, end-stage renal disease and haemodialysis
-
Presented with fever, cough, dyspnoea, bleeding diarrhoea
-
Developed acute left lower quadrant abdominal pain with red bright rectal bleeding
-
PCR positive for SARS-CoV-2
-
Anaemia, leucopoenia, lymphopenia
-
D-dimer level 4226.0 ng/ml; increased ferritin CRP, procalcitonin
-
Thoracic X-rays demonstrated bilateral opacities and abdominal CT-scan suggested ischaemic colitis. Anticoagulant prescribed
-
Stable for 5 days, then cardiac arrest and death
Case 2:
-
Female, 61 years old, with a history of type II diabetes mellitus
-
Three-day history of dry cough and non-radiating abdominal pain for one day
-
Sharp, severe, periumbilical pain which began acutely that morning
-
Positive for SARS-CoV-2
-
Pulmonary angiography CT-scan showed thromboembolism in thoracic + abdominal aorta. D-dimer 8264 ng/ml (>16 times normal)
-
Clinically significant venous and arterial that required tissue plasminogen activator
Implications: COVID-19 associated coagulopathy can include thromboembolism and may present with abdominal pain or pulmonary embolism. In patients with alerting symptoms, increased D-dimer levels should prompt appropriate investigation to detect thrombosis.
Commentary: These are examples of COVID-19 presenting with abdominal pain as presenting symptom. COVID-19 associated coagulopathy can worsen prognosis, because of undetected intestinal ischaemia. D-Dimer is an important investigation if suspect coagulopathy in these patients.
Other cases of COVID-19 related acute-pseudo-surgical abdomen have been reported including;
Ahmed AOE, Badawi M, Ahmed K, Mohamed MFH. COVID-19 Masquerading as an Acute Surgical Abdomen. Am J Trop Med Hyg. 2020 Jun 9.
doi: 10.4269/ajtmh.20-0559. [Epub ahead of print]
Reviewed by EFIC on June 5, 2020 – Read the full article here
Temporomandibular Disorders and Bruxism Outbreak as a Possible Factor of Orofacial Pain Worsening during the COVID-19 Pandemic-Concomitant Research in Two Countries. (J. Clin. Med. 2020 Oct.)
Read the full article here.
The early influence of COVID-19 pandemic-associated restrictions on pain, mood, and everyday life of patients with painful polyneuropathy. (Pain Rep. 2020 Oct.)
Read the full article here.
Perspectives of patients with rheumatic diseases in the early phase of COVID-19 (Arthritis Care & Research, 2020 Sep.)
Type of study: Online survey of rheumatology patients
Level of evidence: Level 4 (Case series or poor quality cohort or case-control study)
Population: Rheumatological patients at a large tertiary hospital in Australia
Methodological approach: People were invited to complete a survey that assessed their concerns regarding risks conferred by their rheumatological condition or medications, impact of receiving information about on the likelihood of continuing medication during the COVID-19 pandemic, and acceptance of telehealth.
Results: The response rate was 21% (550/2630 people). Most people (63.8%) were prescribed more than one conventional synthetic disease-modifying antirheumatic drug and 17.8% were prescribed a biologic or targeted synthetic anti-rheumatic drug. Prednisolone and non-steroidal anti-inflammatory drugs (NSAIDs) use was reported by 26.7% and 22.4% of people, respectively.
41% of people were concerned that their rheumatological disease increased their risk of COVID-19 infection and severity of infection (52.3%). More people were concerned that their medications increased their risk of COVID-19 infection (55.7%), while 76.1% were concerned that medications increased the severity of infection.
Most people (61%) had been provided with information about the impact of COVID-19 on rheumatological conditions. Telehealth was considered appropriate to almost all people (98.4%) during the pandemic.
Commentary: This article exemplifies concerns that either rheumatological conditions and/or their medication might increase the risk for COVID-19 and its severity. Understandably some people may consider stopping their medicines and run the risk of subsequent complications or worsening of their underlying disease.
Reviewed by EFIC on June 12, 2020 – Read the full article here
Characteristics, symptom management and outcomes of 101 patients with COVID-19 referred for hospital palliative care (Journal of Pain and Symptom Management. 2020 Jul.)
Type of study: retrospective analysis of 101 medical and nursing case notes by clinician-researchers
Level of evidence: Level 4 (case series)
Results: Of the 101 patients with COVID-19 infection referred for end-of-life palliative care 64 were males and 37 females with a median age of 82 [72-89]. The most prevalent symptoms were in descendent order breathlessness, agitation, drowsiness, pain, and delirium. Apart from non-pharmacological treatment, patients received mainly symptom-relieving drugs with a median final dose of 10 mg/24 h morphine and 10 mg/24 h midazolam. Patients spent a median of 2 [1–4] days under the palliative care team and received 3 [2–5] contacts. 75 patients died, 13 were discharged and 13 remained under palliative inpatient care.
Implications: This retrospective analysis of a case series of COVID-19 patients receiving end-of-life palliative care instead of a referral to an intensive care ward gives some interesting insights into the course of the disease, the main symptoms under which the patients suffer, the required treatment measures, and their effectiveness.
Commentary: Intriguing is the information on end-of-life palliative care patients with COVID-19 infection in comparison to the intensive care patients that receive much more media attention. However, it provides little new information for the commonly known palliative care. The therapies that were initiated belong to the standard of care.
Reviewed by EFIC on April 30, 2020 – read the full article here.
Guillain-Barré syndrome associated with leptomeningeal enhancement following SARS-CoV-2 infection. (Clin Med (Lond). 2020 Jul.)
Read the full article here.
The Effect of the COVID-19 Pandemic on Electively Scheduled Hip and Knee Arthroplasty Patients in the United States (The Journal of Arthroplasty. 2020 Jul.)
Type of study: Survey
Level of evidence: 2C (Ecological study)
Population: Patients awaiting elective hip and knee arthroplasty
Intervention: A survey (electronically or over the phone) to patients awaiting hip or knee replacement to assess pain, anxiety, physical function and economic capacity to undergo a delayed surgery.
Results: Hospitals in the United States – similar to hospitals in many other countries– stopped performing elective procedures when COVID-19 was declared a pandemic. This led to the deferral of a large number of hip and knee arthroplasties between March and July 2020 and increasing waiting times. Six institutions distributed the survey and 360 patients responded.
Most patients were anxious about the uncertainty of when their deferred surgery would take place. While 85% of the sample agreed with the surgery deferral in line with public health advice, 90% planned to reschedule their surgery as soon as possible. Patients in North East States were most concerned with contracting COVID-19 during their hospital admission. Younger patients were more anxious about the financial situation and job security and its impact on being able to afford the cost of the future surgery.
Implications: The COVID-19 pandemic has a significant impact on patients with hip and knee osteoarthritis who have to wait in uncertainty until their surgery is rescheduled. Supporting individuals during this time with managing pain is very important in terms of both physical and emotional wellbeing.
Commentary: This small survey offers an insight into the impact that COVID-19 is having on patients with knee and hip osteoarthritis who require surgery. The result that 90% of the sample will reschedule their surgery as soon as possible is interesting in light of debate on social media that COVID-19 might lead to a reduction in the number of musculoskeletal pain procedures. A limitation of this study is that it does not reveal how many individuals received the survey, so we are unable to assess the response rate.
Reviewed by EFIC on August 11, 2020 – Read the full article here
Superior Mesenteric Artery Thrombosis and Acute Intestinal Ischemia as a Consequence of COVID-19 Infection. (Am J Case Rep. 2020 Jul.)
Read the full article here.
The emerging spectrum of COVID-19 neurology: clinical, radiological and laboratory findings (Brain. 2020 Jul.)
Type of study: Case series
Level of evidence: 4 (Case series)
Population: Patients with COVID-19 presenting with neurological syndromes
Results: Clinical and paraclinical data collected from 43 consecutive cases with COVID-19 confirmed through RNA PCR, or with probable/possible disease according to World Health Organization criteria, and presenting with neurological symptoms. Five major categories are described:
- (i) encephalopathies (n= 10) with delirium/psychosis and no distinct MRI or CSF abnormalities, with 9 patients making a full or partial recovery with supportive care only;
- (ii) inflammatory CNS syndromes (n= 12) including encephalitis, acute disseminated encephalomyelitis, and isolated myelitis. Of these, 10 were treated with corticosteroids, and one patient died;
- (iii) ischaemic strokes (n= 8) associated with a pro-thrombotic state (four with pulmonary thromboembolism), one of whom died;
- (iv) peripheral neurological disorders (n= 8), seven with Guillain-Barré syndrome, one with brachial plexopathy, six making an ongoing recovery; and
- (v) miscellaneous central disorders (n=5) who did not fit the categories above.
Implications: Such syndromes have similarities to those described in the other coronavirus epidemics (severe acute respiratory syndrome (SARS) in 2003, and Middle East acute respiratory syndrome (MERS) in 2012). However, overall numbers of infected individuals were much smaller, and neurological presentations were few in comparison with those being recognized in the current pandemic.
Commentary: This is probably the most detailed clinical report on the nature of neurological syndromes associated with COVID-19. To be contrasted with the previous report from the Strasbourg group (Helms et al NEJM 2020) who described essentially encephalopathy with agitation, confusion and corticospinal tract signs in 64 patients, as well other less comprehensive reports (Guan et al. NEJM 2020; Mao et al. JAMA Neurol 2020; Varatharaj et al., Lancet Psych 2020).
Reviewed by EFIC on August 11, 2020 – Read the full article here
COVID-19 gastrointestinal symptoms mimicking surgical presentations. (Ann Med Surg (Lond). 2020 Jun.)
Read the full article here.
COVID-19 presenting as severe, persistent abdominal pain and causing late respiratory compromise in a 33-year-old man. (BMJ Case Rep. 2020 Jun.)
Read the full article here.
Adverse effects of COVID-19-related lockdown on pain, physical activity and psychological well-being in people with chronic pain. (Br. J. Pain. 2020.)
Read the full article here.
Rehabilitation & Long COVID
Clinical effectiveness of an online supervised group physical and mental health rehabilitation programme for adults with post-covid-19 condition (REGAIN study): multicentre randomised controlled trial, BMJ 2024
Read the full article here.
Rehabilitation Interventions for Physical Capacity and Quality of Life in Adults With Post-COVID-19 Condition: A Systematic Review and Meta-Analysis (JAMA Netw Open. September 2023)
Read the full article here.
Towards evidence-based and inclusive models of peer support for long covid: A hermeneutic systematic review (Elsevier. 2023 Mar)
Read the full article here.
Peripheral Neuropathy Evaluations of Patients With Prolonged Long COVID (Neurol Neuroimmunol Neuroinflamm. 2022 Mar)
Read the full article here.
Pain Burden in Post-COVID-19 Syndrome following Mild COVID-19 Infection (J Clin Med. 2022 Jan)
Read the full article here.
Rehabilitative management of post-acute COVID-19: clinical pictures and outcomes (Rheumatol Int . 2021 Dec)
Read the full article here.
Long COVID, a comprehensive systematic scoping review (Infection. 2021 Dec)
Read the full article here.
Post-Covid-19 Syndrome: Improvements in Health-Related Quality of Life Following Psychology-Led Interdisciplinary Virtual Rehabilitation ( J Prim Care Community Health . Jan-Dec)
Read the full article here.
Incidence, co-occurrence, and evolution of long-COVID features: A 6-month retrospective cohort study of 273,618 survivors of COVID-19 (Plos Med. 2021 Sep)
Read the full article here.
Long COVID in children and adolescents. (World J Pediatr. 2021 Sep)
Read the full article here.
Characterizing long COVID in an international cohort: 7 months of symptoms and their impact. (EClinicalMedicine. 2021 Aug)
Read the full article here.
Symptoms, complications and management of long COVID: a review (J Roy Soc Med. Jul 2021)
Read the full article here.
Long covid—mechanisms, risk factors, and management (BMJ 2021)
Read the full article here.
Living with long Covid: some reflections 14 months down the line (Évid Based Nurs ebnurs. 2021)
Read the full article here.
Patients' Experiences of "Long COVID" in the Community and Recommendations for Improving Services: A Quality Improvement Survey. (J. of Primary Care & Community Health. 2021 Jan)
Read the full article here.
Returning to physical activity after covid-19. (BMJ. 2021 Jan.)
Read the full article here.
The Stanford Hall consensus statement for post-COVID-19 rehabilitation. (Br J Sports Med. 2020 Aug.)
Read the full article here.
Pain Treatments & Services
Pandemic impact and adaptation to telehealth in chronic pain treatment providers across two COVID-19 pandemic years (Pain Practice. 2024 Feb)
Read the full article here.
Experiences of Pediatric Pain Professionals Providing Care during the COVID-19 Pandemic: A Qualitative Study (Children. 2022 Feb)
Read the full article here.
Understanding the impact of the Covid-19 pandemic on delivery of rehabilitation in specialist palliative care services: An analysis of the CovPall-Rehab survey data. (Palliat Med. 2022 Feb)
Read the full article here.
Substitution of Nonpharmacologic Therapy With Opioid Prescribing for Pain During the COVID-19 Pandemic (JAMA Netw Open. 2021 Dec)
Read the full article here.
A Delphi Consensus Approach for the Management of Chronic Pain during and after the COVID-19 Era (Int J Environ Res Public Health . 2021 Dec)
Read the full article here.
Wahrnehmungen zum Umgang mit Opioiden bei COVID-19 (Der Schmerz. 2021)
Read the full article here.
Impact of the COVID-19 pandemic on corticosteroid injection services: A National Survey of Members of the British Society of Skeletal Radiologists (BSSR). (Br J Radiol. 2021 Oct)
Read the full article here.
Pain Management Nurses’ Roles During the COVID-19 Pandemic (Pain Manag Nurs. 2021 Oct )
Read the full article here.
Efficacy of the FIBROWALK Multicomponent Program Moved to a Virtual Setting for Patients with Fibromyalgia during the COVID-19 Pandemic: A Proof-of-Concept RCT Performed Alongside the State of Alarm in Spain (Int J Environ Res Pu. 2021)
Read the full article here.
Innovation in a Crisis: Lessons Learned from the Rapid Development of an End-of-Life Palliative Care Unit during the COVID-19 Pandemic. (J Palliat Med. 2021 Sep)
Read the full article here.
NSAIDs and COVID-19: A Systematic Review and Meta-analysis ( Drug Saf. Sep 2021)
Read the full article here.
Should we be concerned when COVID-19-positive patients take opioids to control their pain? Insights from a pharmacological point of view (Eur Rev Med Pharmacol Sci. 2021)
Read the full article here.
Nonsteroidal anti-inflammatory drugs and glucocorticoids in COVID-19 (Adv Biol Regul. Aug 2021)
Read the full article here.
Musculoskeletal steroid injections during the COVID-19 pandemic (J Orthop. Aug 2021)
Read the full article here.
Impact of the COVID-19 pandemic on end of life care delivery in care homes: A mixed method systematic review (Palliative Med. 2021)
Read the full article here.
Intravenous Ketamine for Cancer Pain Management, Including Flares During the COVID-19 Pandemic: A Retrospective Study ( Pain Med. Jul 2021)
Read the full article here.
The COVID-19 Vaccine and Interventional Procedures: exploring the relationship between steroid administration and subsequent vaccine efficacy (Pain Pract. 2021 Jul)
Read the full article here.
[Influence of the corona pandemic on pain patients : Which impacts of the pandemic on their care do patients with chronic pain experience?] (Schmerz. 2021 Jun)
Read the full article here.
Intravenous Ketamine for Cancer Pain Management Including Flares During the COVID-19 Pandemic: A Retrospective Study (Pain Med . 2021 Jun)
Read the full article here.
Palliative Care Practice During the COVID-19 Pandemic: A Descriptive Qualitative Study of Palliative Care Clinicians (J Pain Symptom Manag. 2021)
Read the full article here.
Pharmacological strategies used to manage symptoms of patients dying of COVID-19: A rapid systematic review. (May 2021)
Read the full article here.
Patients with Chronic Pain Prefer Maintenance of Pain Treatment Despite COVID-19 Pandemic Restrictions (Pain Physician 2021)
Read the full article here.
COVID-19 Pandemic Impact and Response in Canadian Pediatric Chronic Pain Care: A National Survey of Medical Directors and Pain Professionals (May 2021)
Read the article here.
Interventional Pain Training using Phantom Model during COVID-19 Pandemic (May 2021)
Read the full article here.
Do Corticosteroid Injections for the Treatment of Pain Influence the Efficacy of Adenovirus Vector-Based COVID-19 Vaccines? (Pain Med April 2021)
Read the full article here.
The Use of Remote Programming for Spinal Cord Stimulation for Patients With Chronic Pain During the COVID-19 Outbreak in China (April 2021)
Read the full article here.
Inter-Institutional pain learning exchange (PLEX): Virtual opportunities for learning and collaboration in chronic pain fellowships during the COVID-19 pandemic and beyond (Apr 2021)
Read the full article here.
Symptom management of COVID-19 positive patients in an acute NHS trust: a specialist palliative care team perspective ( Clin Med (Lond). 2021 Mar)
Read the full article here.
Public Interest in Knee Pain and Knee Replacement during the SARS-CoV-2 Pandemic in Western Europe (J Clin Med 2021)
Read the full article here.
Public interest in musculoskeletal symptoms and disorders during the COVID-19 pandemic (Mar 2021)
Read the full article here.
Recommendations and Guidance for Steroid Injection Therapy and COVID-19 Vaccine Administration from the American Society of Pain and Neuroscience (ASPN) (Mar 2021)
Read the full article here.
Pain management in COVID-19 pediatric patients-An evidence- based review ( Saudi J Anaesth Jan-Mar 2021)
Read the full article here.
Quantifying the impact of COVID-19 on chronic pain services in the Republic of Ireland. (Ir J Med Sci. 2021 Feb.)
Read the full article here.
Neuro-axial steroid injection in pain management and COVID-19 vaccine. (Eur J Pain. 2021 Feb.)
Read the full article here.
Use of non-steroidal anti-inflammatory drugs and risk of death from COVID-19: an OpenSAFELY cohort analysis based on two cohorts. (Ann Rheum Dis. 2021 Jan.)
Read the full article here.
Chronic Pain and COVID-19: pathophysiological, clinical and organizational issues. (Minerva Anestesiol. 2020 Dec.)
Changes in Interventional Pain Physician Decision-Making, Practice Patterns, and Mental Health During the Early Phase of the SARS-CoV-2 Global Pandemic. (Pain Med. 2020 Dec.)
Read the full article here.
. Pain in the Pandemic: Ethical Approaches During COVID-19. (Pain Med. 2020 Nov.)
Read the full article here.
How to Restart the Interventional Activity in the COVID-19 Era: The Experience of a Private Pain Unit in Spain. (Pain Pract. 2020 Nov.)
Read the full article here.
Pain Management During the COVID-19 Pandemic in China: Lessons Learned (Pain Medicine. 2020 Nov.)
Type of article: Case reports from physicians about managing pain during the COVID-19 pandemic
Level of evidence: 5 (Expert opinion without critical appraisal or based on physiology bench research or first principles
Results: Most medical services In Wuhan not directly involved in intensive care, including pain management services, were partially or completely shut down. This posed challenges for clinicians and people with chronic pain. The pain medicine department found that widespread pain can be an early symptom of COVID-19 infection.
On the other hand, an increasing concern is that the concern of missing other urgent medical conditions or diagnoses when focusing on assessing for COVID-19 infection. A case of thoracic spinal neuratoma left undiagnosed due to similarities in presentation to COVID-19 infection is reported. The pandemic provided clinicians an opportunity to incorporate telemedicine into pain management for the first time due to the urgent need to provide healthcare services remotely. Clinicians need to consider strategies to encourage people with health issues needing management to seek outpatient care as many are still understandably wary of seeking in-person health care. We may prepare ourselves to see more patients who previously had COVID-19 infection visiting pain clinic as the epidemic slows.
Commentary: As well as clinical research, personal experiences in the pandemic are be important to share too. The included case reports illustrate how the combination of chronic pain and COVID-19 infection can challenge diagnosis and treatment.
Beneficial strategies for managing pain during the COVID-19 pandemic are reported and recommendations based on lessons learned in the pain medicine departments of Wuhan and Shenzhen hospitals are discussed.
Reviewed by EFIC on May 8, 2020 – read the full article here.
Non-steroidal anti-inflammatory drugs, prostaglandins, and COVID-19. (Br J Pharmacol. 2020 Nov.)
Read the full article here.
Pain management programmes via video conferencing: a rapid review. (Scand J Pain. 2020 Oct.)
Read the full article here.
Impact of COVID-19 on chronic pain patients: a pain physician's perspective. (Pain Manag. 2020 Sep.)
Read the full article here.
Adverse outcomes and mortality in users of non-steroidal anti-inflammatory drugs who tested positive for SARS-CoV-2: A Danish nationwide cohort study (Plos Medicine. 2020 Sep.)
Type of study: Cohort study
Level of evidence: 2B (individual cohort study)
Population: All Danish residents who tested positive for the infectious agent of COVID-19. A total of 9,236 SARS-CoV-2 PCR-positive individuals were eligible for inclusion.
Intervention: Users of NSAIDs (248 (2.7%) had filled a prescription for NSAIDs)
Comparison: Non-users of NSAIDs
Results: Treatment with NSAIDs was not associated with 30-day mortality, risk of hospitalization, ICU admission, mechanical ventilation or renal replacement therapy.
Implications: Use of Danish registries allowed for identification of all individuals who had been tested for SARS-CoV-2 in Denmark and allowed for obtaining data on prescription drug use, medical history, migration, hospital admissions, and death through individual-level linkage between health and administrative registries. The main limitations of the study are possible exposure misclassification, as not all individuals who fill an NSAID prescription use the drug continuously, and possible residual confounding by indication, as NSAIDs may generally be prescribed to healthier individuals due to their side effects, but on the other hand may also be prescribed for early symptoms of severe COVID-19.
Considering the available evidence, there is no reason to withdraw well-indicated use of NSAIDs during the SARS-CoV-2 pandemic. However, the well-established adverse effects of NSAIDs, particularly their renal, gastrointestinal, and cardiovascular effects, should always be considered, and NSAIDs should be used in the lowest possible dose for the shortest possible duration for all patients.
Commentary: This is a large cohort study demonstrating that NSAIDs do not lead to more severe coronavirus disease. This is an important finding as different theories on the use of NSAIDs were proposed during the early phases of the COVID-19 pandemic where concerns were raised that NSAIDs may lead to a more severe course of coronavirus disease.
Reviewed by EFIC on September 21, 2020 – Read the full article here
COVID-19 impact and response by Canadian pain clinics: A national survey of adult pain clinics (Sep 2020)
Read the full article here
Corticosteroid Injections and COVID-19 Infection Risk. (Pain Med. 2020 Aug.)
Read the full article here.
Clinical and economic strategies in outpatient medical care during the COVID-19 pandemic. (Reg Anesth Pain Med. 2020 Aug.)
Read the full article here.
Emergence From the COVID-19 Pandemic and the Care of Chronic Pain: Guidance for the Interventionalist. (Anesth Analg. 2020 Aug.)
Read the full article here.
Managing chronic pain patients at the time of COVID-19 pandemic. (Minerva Anestesiol. 2020 Aug.)
Read the full article here.
Availability of Internationally Controlled Essential Medicines in the COVID-19 Pandemic. (J Pain Symptom Manage. 2020 Aug.)
Read the full article here.
Palliative care for patients with severe covid-19. (BMJ. 2020 Jul.)
Read the full article here.
Home-based management of knee osteoarthritis during COVID-19 pandemic: literature review and evidence-based recommendations (Journal of Experimental Orthopaedics. 2020 Jul.)
Type of study: Review article
Level of evidence: 5 (Narrative systematic review)
Results: Management strategies identified include exercise, proper nutrition, physical therapy, and use of corrective and assistive orthotics.
Telehealth methods may be considered to deliver self-management advice to patients with knee osteoarthritis who had their surgery deferred. Home exercise programmes consisting of a combination of aerobic, resistance, and flexibility work should be considered.
Where patients with knee osteoarthritis have co-morbid obesity, a combined exercise, and diet approach to encourage weight loss can be considered.
The role of knee braces, sleeves, foot orthoses, footwear, walking aids and heat is uncertain in terms of pain, disability, and quality of life.
Commentary: This review article provides an overview of the non-pharmacological options for the home management of knee osteoarthritis. Exercise and virtual education appear to be the most promising interventions with the strongest supporting evidence. However, the review article lacks a risk of bias assessment and pooled analyses and so the true effectiveness of any of the proposed strategies remains uncertain.
Reviewed by EFIC on August 11, 2020 – Read the full article here
NSAIDs in patients with viral infections, including Covid-19: Victims or perpetrators? (Pharmacol Res. 2020 Jul.)
Read the full article here.
Clinicians’ Initial Experiences of Transition to Online Interdisciplinary Pain Rehabilitation During the Covid-19 Pandemic (J Rehabil Med Clin Commun June 2020)
Read the full article here.
COVID-19 pandemic and therapy with ibuprofen or renin-angiotensin system blockers: no need for interruptions or changes in ongoing chronic treatments (Naunyn-Schmiedeberg's Archives of Pharmacology. 2020 May.)
Type of study: Review
Level of evidence: 5 (Expert opinion without critical opinion or based on physiology bench research or first principles)
Results: There remains no scientific evidence establishing a clear link between renin-angiotensin system (RAS) blockers (including angiotensin receptor blockers (ARBs), angiotensin converting enzyme inhibitors ACE-I), or non-steroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen and the worsening of COVID-19. In contrast, experimental data support the idea that ACE-2 not only serves as an entry receptor for SARS-CoV-2 but also protects the lungs from acute injury, and hence may therefore be beneficial in COVID-19 infection.
Implications: The authors propose that effective treatment with RAS blockers should not be discontinued or switched. There is insufficient evidence to recommend patients who take ibuprofen for medically indicated reasons to change their anti-inflammatory medicine in light of the COVID-19 pandemic. The choice of drug to treat COVID-19-associated fever or pain should be based on a benefit-risk assessment considering known side effects (e.g. kidney damage, gastrointestinal ulceration).
Commentary: The hypothetical risk of worsening COVID-19 does not justify discontinuing or switching RAS blockers or ibuprofen. Changes to treatment should be made in the light of benefit-risk assessment of these drugs for individuals.
Reviewed by EFIC on May 20, 2020 – Read the full article here
EMA advice on the use of NSAIDs for Covid-19. (Drug Ther Bull. 2020 May.)
Read the full article here.
Radiotherapy for pain relief from bone metastases during Coronavirus (COVID-19) pandemic (European Journal of Pain. 2020 May.)
Type of article: Letter to the Editor
Population: Patients with cancer pain from bone metastases
Intervention: Radiotherapy for painful bone metastases
Results: Bone metastases are a common complication of advanced cancer that cause spinal cord compression, life-threatening electrolyte imbalances, pathologic fracture and severe pain. Stepwise treatments are opioids/NSAIDs, bisphosphonates, chemo & hormone-therapy, radiation and surgery. Palliative radiotherapy for painful uncomplicated bone metastases yields significant palliation for approximately 70% of people and complete pain relief for 10-35%. In previous RCTs, both single fraction and multiple fraction radiation therapy were efficacious for pain in bone metastases, multiple fraction are better only for patients with complicated metastases, neuropathic pain or cord compression.
In the context of the current COVID-19 epidemic, this choice must be weighted with the infection risks cancer patients due to a compromised immune system. In patients with cord compression and poor survival prognosis, a single fraction of 8 Gy was found as effective as multifractionated regimens while minimizing multiple treatment visits.
Implications: In order to minimize the exposure of people with bone metastases to COVID-19 without compromising oncological outcome, the choice of a palliative radiotherapy with 8 Gy in one single fraction may be the most reasonable, with good efficacy and reduced length of patients’ exposure to hospital environment and contagion.
Commentary: The National Institute for Health and Care Excellence (NICE) in the UK recommended using radiotherapy “only if unavoidable” (Mahase E BMJ. 2020 Apr 1;369:m1338.). In the light of literature, this report recommends the use of single fraction 8 Gy radiotherapy instead of longer schedules as a safer and reasonable procedure for painful bone metastases refractory to pain medication or with spinal cord compression, during the COVID-19 epidemic.
Of particular note, the risks and benefits of radiotherapy should always be discussed with patients and staff, and adequate preventive and protective measures provided to patients and radiotherapy technicians. Radiation treatment room and nearby areas should be sanitized during treatment intervals, and the time patients spend in the waiting room minimised. A dedicated path for cancer patients separated from other hospital patients should be assured.
Reviewed by EFIC on May 20, 2020 – read the full article here
Pain Management Best Practices from Multispecialty Organizations during the COVID-19 Pandemic and Public Health Crises (Pain Medicine. 2020 Apr.)
Type of study: Narrative review
Level of evidence: 5 (Expert opinion without explicit critical appraisal or based on physiology bench research or first principles)
Results: This consensus provides a good overview on safety precautions to reduce risks of infection with SARS-CoV-2 for clinicians working in pain management and the patients they treat. Other issues considered include patient flow issues and staffing plans, telemedicine options, triaging recommendations and resource utilization, and impacts on mental health of both patients and healthcare workers. Guidance on the prescription of opioids and use of steroids for interventions is provided
Commentary: The paper summarises the opinions of an expert panel that included pain management experts from the military, Veterans Health Administration, and academia in the US. Hence, the recommendations reflect current practices in the US and may not be directly applicable in other settings.
Reviewed by EFIC on April 30, 2020 – read the full article here.
Caring for patients with pain during the COVID‐19 pandemic: consensus recommendations from an international expert panel (Anesthesia. 2020 Apr.)
Type of study: Practice recommendations to help with the care of chronic pain patients during the COVID-19 pandemic.
Level of evidence: 5 (Expert opinion without explicit critical appraisal or based on physiology bench research or first principles).
Results: Consensus recommendations on a range of topics including:
- face to face consultations (not recommended)
- telemedicine (recommended providing fits with legislative regulations)
- biopsychosocial management (recommended if social distancing can be maintained or using remote consultations)
- maintain regular review of patients prescribed opioids and that all patients receive their prescription of opioids to avoid withdrawal; and
- patients may continue prescribed NSAIDs for pain relief.
Commentary: The paper gives an overview of the expert opinion of a panel. However, the size of panel not stated. While the quality low, evidence in the paper may provide a benchmark for comparison to any local practice.
Reviewed by EFIC on April 30, 2020 – read the full article here.
The role and response of palliative care and hospice services in epidemics and pandemics: a rapid review to inform practice during the COVID-19 pandemic (Journal of Pain and Symptom Management. 2020 Apr.)
Type of study: A rapid systematic literature review of published case studies, cross-sectional studies, cohort studies, and intervention studies
Level of evidence: Level 3A (Systematic review of case-control studies)
Results: Out of 2207 identified studies, 36 underwent full-text review, and 10 studies were finally selected for analysis.
To guide hospices and palliative care teams they should focus on:
- maintaining the ability to respond rapidly and flexibly;
- ensuring protocols for symptom management and psychological support, and non-specialists are trained in their use;
- being involved in triage;
- considering shifting resources from inpatient to community settings;
- considering redeploying volunteers to provide psychosocial care;
- facilitating camaraderie among staff and adopting measures to deal with stress;
- using technology to communicate with patients and carers; and
- adopting standardised data collection systems to inform operational changes and improve care.
Implications: Palliative care teams need to be flexible and rapidly redeploy resources in the face of changing needs during a pandemic, such as COVID-19. Particular attention should be to the triage of patients, palliative care expertise staff, workload and stress, anticipatory allocation of space and equipment, and standardised documentation of data.
Commentary: This rapid review provides guidance for hospices and palliative care teams to ensure that they do not become overwhelmed by rapid developments of a pandemic. There was limited detail about how studies were selected for undergoing full-text review. In addition, there was only limited evidence and a lack of quantitative data, no assessment of quality of studies, and no grading of recommendations. The use of a developed palliative care surge plan might have been used as a filter for the selection of studies. Despite these limitations, this paper gives a valuable review of literature relevant for palliative care and provides important guidance.
Reviewed by EFIC on April 30, 2020 – read the full text here.
Mechanisms & Science
The uptake and effectiveness of a multidisciplinary online program for managing chronic pain before and during the COVID-19 pandemic (Pain Med. 2022 Mar)
Read the full article here.
Comparison the Effect of Pain Neuroscience and Pain Biomechanics Education on Neck Pain and Fear of Movement in Patients with Chronic Nonspecific Neck Pain During the COVID-19 Pandemic (Pain Ther. 2022 Mar)
Read the full article here.
Perceptions on the use of opioids: focus on COVID-19 : Free-text analysis of a survey in anesthesiology/intensive care, internal medicine, and palliative care (Schmerz. 2022 Jan)
Read the full article here.
Changes in Outpatient Opioid Prescribing During the COVID-19 Pandemic: An Interrupted Time Series Analysis (J Prim Care Community Health. 2022 Jan)
Read the full article here.
Pain catastrophizing mediates rapid benefits of accessing in-person chiropractic care during the COVID-19 lockdown (Eur J Pain. 2021)
Read the full article here.
Chronic Pain in Schoolchildren and its Association With Psychological Wellbeing Before and During the COVID-19 Pandemic (J Adolesc Health. 2021 Nov)
Read the full article here.
Chronic low back pain during COVID-19 lockdown: is there a paradox effect? (Eur Spine J. 2021 Nov)
Read the full article here.
The health-related quality of life of patients with musculoskeletal disorders after the COVID-19 pandemic (Int Orthop. 2021 Nov )
Read the full article here.
Manifestations of Pain during the COVID-19 Pandemic Portrayed on Social Media: A Cross-Sectional Study (Pain Med. 2021 Oct)
Read the full article here.
Experience of the COVID-19 pandemic as lived by patients with hip and knee osteoarthritis: an Italian qualitative study (BMJ Open. 2021 Oct)
Read the full article here.
The Experiences of Individuals Experiencing Pain During COVID-19 Infection: A Phenomenological Study ( Pain Manag Nurs. 2021 Oct)
Read the full article here.
The Relationship between Pain and Psychological Distress during the COVID-19 Pandemic: Is Social Technology Use Protective? (Pain Med. 2021 Sep)
Read the full article here.
Chronic Pain in Schoolchildren and its Association With Psychological Wellbeing Before and During the COVID-19 Pandemic. (J Adolesc Health. 2021 Sep)
Read the full article here.
Time course prevalence of post-COVID pain symptoms of musculoskeletal origin in patients who had survived to SARS-CoV-2 infection: a systematic review and meta-analysis. (Pain. 2021 Sep)
Read the full article here.
1-year outcomes in hospital survivors with COVID-19: a longitudinal cohort study. (Lancet. 2021 Aug)
Read the full article here.
Chronic primary pain in the COVID-19 pandemic: how uncertainty and stress impact on functioning and suffering (Pain. Aug 2021)
Read the full article here.
Expected impact of lockdown measures due to COVID-19 on disabling conditions: a modelling study of chronic low back pain (European Spine Journal. 2021)
Read the full article here.
Rationale and study design of an early care, therapeutic education, and psychological intervention program for the management of post-intensive care syndrome and chronic pain after COVID-19 infection (PAIN-COVID): study protocol for a randomized controlled trial (Trials. Jul 2021)
Read the full article here.
Association between chronic pain medications and the severity and mortality of COVID-19: Study protocol for a case-population study (Medicine (Baltimore). Jul 2021)
Read the full article here.
The Experiences of People Living With Chronic Pain During a Pandemic: "Crumbling Dreams With Uncertain Futures". (Qualitative Health Research. Jun 2021)
Read the full article here.
Central Sensitization Phenotypes in Post Acute Sequelae of SARS-CoV-2 Infection (PASC): Defining the Post COVID Syndrome ( J Prim Care Community Health. July 2021)
Read the full article here.
Rationale and study design of an early care, therapeutic education, and psychological intervention program for the management of post-intensive care syndrome and chronic pain after COVID-19 infection (PAIN-COVID): study protocol for a randomized controlled trial (BMC. 2021 July)
Read the full article here.
Isolated and anxious: A qualitative exploration of the impact of the COVID-19 pandemic on individuals living with spinal cord injury in the UK (J Spinal Cord Med. 2021 Jul)
Read the full article here.
Expected impact of lockdown measures due to COVID-19 on disabling conditions: a modelling study of chronic low back pain ( Eur Spine J . 2021 Jul)
Read the full article here.
Myopathic changes in patients with long-term fatigue after COVID-19 (Clin Neurophysiol. 2021)
Read the full article here.
Cohort study protocol to characterize the incidence and severity of neuropathic pain in patients with severe acute respiratory syndrome coronavirus 2 infection (Pain Reports. 2021)
Read the full article here.
Longitudinal study of early adaptation to the coronavirus disease pandemic among youth with chronic pain and their parents: effects of direct exposures and economic stress (Pain Publish Ahead of Print, 2021).
Read the full article here.
Chronic pain experience and health inequities during the COVID-19 pandemic in Canada: qualitative findings from the chronic pain & COVID-19 pan-Canadian study (Int. J. for Equity in Health. June 2021)
Read the full article here.
Neurology and neuropsychiatry of COVID-19: a systematic review and meta-analysis of the early literature reveals frequent CNS manifestations and key emerging narratives (J Neurology Neurosurg Psychiatry. 2021)
Read the full article here.
A Study of the Effects of the COVID-19 Pandemic on the Experience of Back Pain Reported on Twitter® in the United States: A Natural Language Processing Approach (Apr 2021)
Read the full article here.
Substance use and abuse, COVID-19-related distress, and disregard for social distancing: A network analysis (Addict Behav. 2021 Mar)
Read the full article here.
COVID-19 psychological factors associated with pain status, pain intensity, and pain-related interference ( Cogn Behav Ther. Feb 2021)
Read the full article here.
A clinical primer for the expected and potential post-COVID-19 syndromes. (Pain Rep. 2021 Feb.)
Read the full article here.
Neurobiology of SARS-CoV-2 interactions with the peripheral nervous system: implications for COVID-19 and pain. (Pain Rep. 2021 Jan.)
Read the full article here.
Potential for increased prevalence of neuropathic pain after the COVID-19 pandemic. (Pain Rep. 2021 Jan.)
Read the full article here.
Considering the potential for an increase in chronic pain after the COVID-19 pandemic. (Pain. 2020 Aug.)
Read the full article here.
COVID stress syndrome: Concept, structure, and correlates (Depress Anxiety. 2020 Jul)
Read the full article here.
A contextual-behavioral perspective on chronic pain during the COVID-19 pandemic and future times of mandated physical distancing. (July 2020)
Read the full article here.
Development and initial validation of the COVID Stress Scales (J Anxiety Disord. 2020 May)
Read the full article here.
Telemedicine
Is Telerehabilitation a Viable Option for Patients with Low Back Pain? Associations between Telerehabilitation and Outcomes during the COVID-19 Pandemic (Phys Ther. 2022 Feb)
Read the full article here.
Management of Chronic Disease in Pandemic Situations: Teleconsultation in Patients with Chronic Pain (Pain Med. 2021 Dec)
Read the full article here.
Chronic Pain Treatment and Digital Health Era-An Opinion (Front Public Health. 2021 Dec)
Read the full article here.
Telemedicine for chronic pain treatment during the COVID‐19 pandemic: Do pain intensity and anxiousness correlate with patient acceptance? (Pain Pract. 2021 Nov)
Read the full article here.
Telehealth Increases Access to Brief Behavioral Interventions in Orofacial Pain Clinic during COVID-19 Pandemic: A Retrospective Study (Pain Med. 2021 Oct)
Read the full article here.
Telemedicine in rheumatology: high specificity and sensitivity of follow-up virtual video consultations during COVID-19 pandemic (Rheumatology (Oxford). Aug 2021)
Read the full article here.
Telehealth and Pain Management (Pain Manag Nurs. Aug 2021)
Read the full article here.
Telehealth: rapid adoption in community palliative care due to COVID-19: patient and professional evaluation ( BMJ Support Palliat Care. 2021 Jun)
Read the full article here.
Best practices for virtual care to support youth with chronic pain and their families: a rapid systematic review to inform health care and policy during COVID-19 and beyond (Pain Reports, 2021)
Read the full article here.
Headache teleconsultation in the era of COVID-19: Patients' evaluation and future directions (Eur J Neurol. 2021)
Read the full article here.
Rapid evidence and gap map of virtual care solutions across a stepped care continuum for youth with chronic pain and their families in response to the COVID-19 pandemic. (Pain. May)
Read the full article here.
Enablers and barriers of people with chronic musculoskeletal pain for engaging in telehealth interventions: protocol for a qualitative systematic review and meta-synthesis (Pain Publish Ahead of Print, 2021)
Read the full article here.
Uptake of Tele-Rehabilitation in Finland amongst Rehabilitation Professionals during the COVID-19 Pandemic (Apr 2021)
Read the full article here.
Telehealth and chronic pain management from rapid adaptation to long-term implementation in pain medicine: A narrative review (Pain Reports. Feb 2021)
Read the full article here.
Optimizing telehealth pain care after COVID-19. (Pain. 2020 Nov.)
Read the full article here.
Telehealth for musculoskeletal physiotherapy (Musculoskeletal Science and Practice. 2020 Aug.)
Type of study: Masterclass / non-systematic overview
Level of evidence: 5 (Expert opinion)
Results: Telehealth is defined as the ‘delivery of healthcare at a distance using information and communication technology’. Published systematic reviews shows that delivering interventions via telehealth methods yield similar effects on pain and disability as face to face interventions in patients with low back pain and hip/knee osteoarthritis. This is based on low certainty evidence and higher-quality trials are required.
A systematic review [Mani S et al. J Telemed Telecare 2017; 23(3): 379–391] found that telehealth assessments have good concurrent validity for pain, swelling, range of motion, muscle strength, balance, gait and functional assessment. However, only low to moderate concurrent validity was demonstrated for special orthopaedic tests, neurodynamic tests, and lumbar posture.
There is high satisfaction with telehealth interventions among individuals with musculoskeletal conditions. Patient barriers to engaging with telehealth include computer literacy, older age, lower education levels, and lack of trust in the clinician. Physiotherapist barriers to engaging with telehealth include unwillingness to change current clinical practice, low confidence with technology, and concerns over safety and patient privacy.
When choosing a telehealth platform, physiotherapists should consider components needed for their assessment (e.g. range of motion features), national privacy and security regulation for the transfer and storage of patient information, usability for the patient, cost, functionality (can be used across different browsers and has multiple features including appointment scheduling).
Implications: Telehealth seems a useful alternative to face to face consultations and interventions in terms of effectiveness for treating musculoskeletal pain conditions.
Commentary: This paper provides a useful overview of the current evidence base for the effectiveness of telehealth interventions for the treatment of pain and disability among patients with musculoskeletal conditions. The paper highlights the results of published systematic reviews showing that telehealth interventions provide similar effects to face to face rehabilitation.
The authors specifically mention the limitations in the evidence base and call for the conduct of high-quality trials before any definitive conclusions can be drawn. The paper outlines very practical tips for picking a telehealth platform and implementing telehealth in physiotherapy practice.
Reviewed by EFIC on August 11, 2020 – Read the full article here
Experience of telemedicine use in a big cohort of patients with rheumatoid arthritis during COVID-19 pandemic ( Ann Rheum Dis 2020 Jun)
Read the full article here
Managing patients with chronic pain during the COVID-19 outbreak: considerations for the rapid introduction of remotely supported (eHealth) pain management services. (Pain. 2020 May.)
Read the full article here.
Webinars
The EFIC COVID-19 Task Force, regularly hold Webinars on themes related to COVID-19 and Pain, feel free to watch them below!
SUMMARIES
Long COVID Webinar
The inaugural COVID webinar focussed on the patient experience of living with long COVID. Dr Ian Frayllng described the significant the impact it has had on his ability to function and work. Dr Andreas Kopf described the German approach to the referral, assessment and management of patients with this condition.
COVID-19 and Rehabilitation Webinar
The second COVID webinar reflected on rehabilitation for COVID-19 and its future in a post-COVID world. Dr Derick T Wade focussed his presentation on post COVID problems, rehabilitation processes, services and organisation and Femke Driehuis, discussed physiotherapy in patients with COVID-19, the role of physiotherapy and and key recommendations when it comes to acute hospital setting and after hospital admission or illness at home.
Additional Resources
Please see the following resources for more research on COVID-19:
- BMJ: https://www.bmj.com/coronavirus
- British Journal of Anaesthesia: https://bjanaesthesia.org/COVID-19-and-the-anaesthetist
- Elsevier: https://www.elsevier.com/connect/coronavirus-information-center
- The Lancet: https://www.thelancet.com/coronavirus
- NEJM: https://www.nejm.org/coronavirus
- SAGE journals: https://journals.sagepub.com/coronavirus
- Springer Nature: https://www.springernature.com/gp/researchers/campaigns/coronavirus
- Wiley: https://novel-coronavirus.onlinelibrary.wiley.com
- Wolters Kluwer for Clinicians: http://tools.ovid.com/coronavirus/
- Wolters Kluwer: http://healthclarity.wolterskluwer.com/coronavirus-resources.html
- WHO: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/global-research-on-novel-coronavirus-2019-ncov
- EU/OSHA:
SURVEYS
‘The Impact of COVID-19 on clinical pain services’
The European Pain Federation EFIC, developed in 2022 a survey on the impact of COVID-19 on clinical pain services and the adjustments made as a consequence. There were two versions of the survey, one targeted at service providers and one targeted at service users. The questions referred to the experience of “telehealth” visits: healthcare appointments that were provided over the telephone or videoconferencing software, amogst other pain and COVID-19 related questions. Both surveys were comparable, in order to draw conclusions afterwards. The results of the survey will be made available in this page shortly!
‘The Effects of COVID-19 on Pain Management Throughout Europe’
The European Pain Federation conducted a survey (April 2020), on ‘The effects of COVID-19 on pain management throughout Europe’. We have summarised the key findings from the survey and have produced a multi-page infographic to illustrate the results. Please contact secretary@efic.org if you wish to use these materials for your own campaign activities, or if you wish to request a translation into your own local language. This resource may also be used for educational and/or informative purposes.
Download the brochure here.