Press Area
The European Pain Federation EFIC welcomes the interest of press in issues related to pain research and medicine. Please find a collection of press materials on current issues below.
2023
The Future of European Pain Research
Press Statement
The Future of Pain Research in Europe
- Chronic pain is the number one reason why people seek healthcare, accounting for over 50% of sickness absences and 60% of permanent disabilities in Europe alone
- Pain research in Europe is making important strides; however, greater investment and collaboration will be needed to continue to improve the lives of those affected by pain.
- The European pain science community are now finalising research priorities that should be taken forward by policy makers, funders, and research institutions directly.
Brussels, 22 March 2023 – On 21 March 2023, experts from the European Pain Federation EFIC and the IMI-PainCare consortium were invited to share their insights at a panel discussion on “The Future of European Pain Research” co-hosted by MEPs Cristian Silviu Busoi and Alex Agius Saliba and attended by representatives from the European Cancer Organisation, European Brain Council, Innovative Health Initiative, European Association for Palliative Care, World Physiotherapy (Europe region), European Federation of Psychologists’ Associations and European Society of Anaesthesiology and Intensive Care.
Chronic pain has a huge societal burden: It is the number one reason why people seek healthcare and is a leading cause of disability worldwide, accounting for over 50% of sickness absences and 60% of permanent disabilities in Europe alone, often leading to significant decreases in quality of life and high healthcare costs. An estimated 100 million people suffer from chronic pain in Europe, with conditions ranging from back pain and arthritis to neuropathic pain and migraines.
“The burden of chronic pain on individuals, families, and societies cannot be underestimated,” said Brona Fullen, President of the European Pain Federation. “We need to develop new approaches to understanding and treating chronic pain if we are to improve the lives of millions of people across Europe and beyond.”
The European Pain Federation EFIC, a multidisciplinary professional organization in the field of pain research and medicine, sees the urgent need to focus on these key areas in pain research:
- Understanding pain: Knowledge of the causes of chronic pain, and how it emerges, is still limited.
- Assessing and diagnosing pain: Better pain measurement tools for different patient groups will lead to more accurate, and early, diagnoses.
- Development of new treatments: Most current treatments for chronic pain have only modest short-term benefits.
- Increase use of effective and safe treatments and reduce use of ineffective and harmful treatments: There is an underuse of treatments that can help people safely and effectively; at the same time, many people receive treatments that do not work and that carry harms.
- Personalised pain management: Current treatments are one-size-fits-all in nature, and are not individualised to the patient’s gender, age, lifestyle or overall health.
- Understand and address comorbidities: Pain is often co-existent with other health conditions, including mental health disorders, obesity, and sleep disorders – all of which complicate management and slow recovery.
- Assess and target patient health literacy: People with a lived experience of chronic pain often receive health information that is difficult to understand and act on and are rarely involved in efforts to improve pain knowledge, practice, and policy.
IMI-PainCare is part of the Innovative Medicines Initiative (IMI), a public-private partnership between the European Union and the pharmaceutical industry aiming to advance medical research and improve healthcare by bringing together stakeholders from different sectors to collaborate on research projects. While pain research, such as IMI-PainCare, is currently funded by the European Union, the European pain science community are now finalising research priorities that should be taken forward by policy makers, funders, and research institutions directly.
In conclusion, pain research in Europe is making important strides in understanding the underlying mechanisms of pain and developing new treatments and therapies. However, there is still much work to be done, and greater investment and collaboration will be needed to continue to advance our understanding of this complex condition and improve the lives of those affected by pain.
About the European Pain Federation EFIC:
The European Pain Federation EFIC is a multidisciplinary professional organization in the field of pain research and medicine, consisting of the 38 European Chapters of the International Association for the Study of Pain (IASP) and representing some 20,000 physicians, nurses, scientists, psychologists, physiotherapists, and other health care professionals involved in pain medicine.
For more information about the European Pain Federation EFIC and its vision for the future of pain research in Europe, please visit this website or contact Executive Director Sam Kynman directly at sam.kynman@efic.org.
Additional Resources
Impressions from the Event









2021
European Clinical Practice Recommendations on Opioids for Chronic Non-Cancer Pain
Press Statement
European scientific community publishes consensus recommendations on opioid use for chronic non-cancer pain
- To allay concerns over an opioid crisis, as in the US, the European scientific community has reviewed evidence on using opioids to treat chronic non-cancer pain
- New clinical practice recommendations have been developed and endorsed by nine leading scientific societies and Europe’s leading pain patients’ organisation
- Recommendations propose opioids should not be prescribed for many chronic pain conditions, and serve only as a second- or third-line treatment in all others
Brussels, 3 March 2021 – Under the umbrella of the European Pain Federation (EFIC), a gathering of nine European scientific societies and a leading patients’ organisation has developed new clinical recommendations for opioid use in treating chronic non-cancer pain (CNCP).
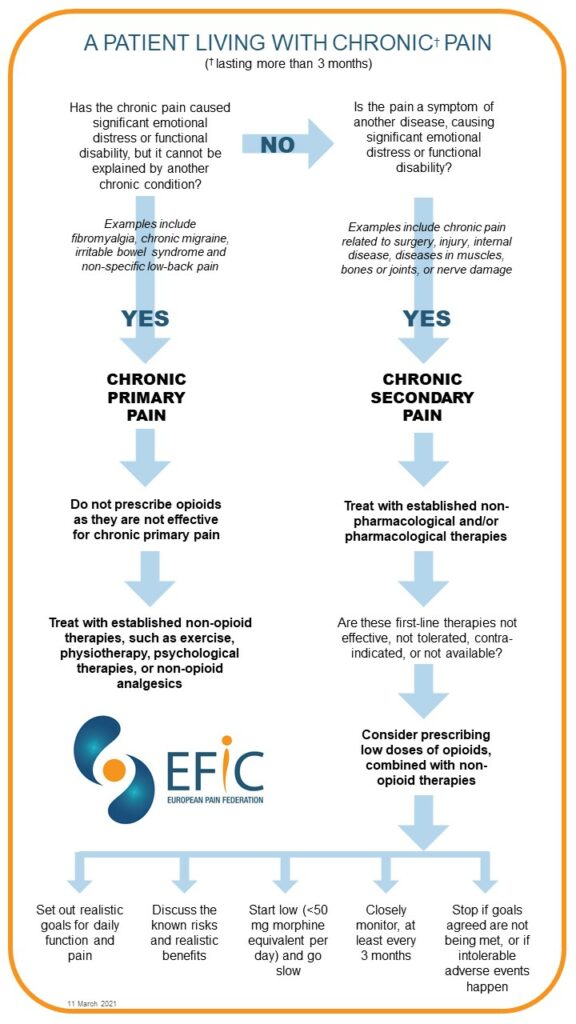
The new recommendations advise that opioids should not be prescribed for people with chronic primary pain as they do not work for these patients. Moreover, opioids should also not be used as a ‘first-line therapy’ for chronic secondary pain syndromes. Instead, doctors should first use non-opioid medications, or established non-pharmacologic therapies (eg exercise, psychological therapies), and only consider prescribing opioids if these first-line therapies do not work, are not tolerated, or contra-indicated.
Chronic primary pain is defined by the World Health Organisation as pain that lasts more than three months, causing significant emotional distress or functional disability, but which cannot be explained by another specific medical condition. Examples include fibromyalgia, chronic migraine, irritable bowel syndrome and non-specific low-back pain. Chronic secondary pain, by contrast, is pain due to a defined medical condition, such as following surgery or injury, internal diseases, diseases of the muscles, bones or joints, or nerve damage.
Up to a quarter of Europeans suffer chronic pain and, in around 80% of those cases, the pain is not related to cancer. In the past, opioids have frequently been prescribed for CNCP because people assume they are the most potent pain medication, coupled with a lack of awareness about the potential serious harm resulting from taking opioids.
Opioid prescriptions have increased over the past decade in some European countries which has caused concerns. The new recommendations therefore aim to provide safer and more effective care for people with CNCP, to improve communication between clinicians and people with chronic pain about the benefits and harms of using prescription opioids for chronic pain, and to give guidance to doctors on appropriate opioid use as well as decrease harmful opioid use.
The recommendations state that, before prescribing opioids, clinicians should establish treatment goals with patients, including realistic goals for daily physical function and pain. In addition, before starting – and regularly throughout the opioid therapy – doctors should discuss the known harms and realistic benefits of opioid therapy (and of alternatives) with their patients. And if opioids are used to treat chronic secondary pain, they should always be combined with non-opioid pain killers and non-opioid therapies.
Doctors should closely monitor patients after starting treatment with opioids and the therapy should only continue if there is clinically meaningful improvement in pain and physical function that outweighs the risks to their patient’s safety.
EFIC’s new recommendations advise starting low and going slow. At the outset, clinicians should prescribe the lowest effective dose: less than 50 morphine milligram equivalents (MME) a day. They should also avoid increasing the dosage above 90 MME/day, or carefully justify any decision to do so.
Opioid therapy should stop if the goals agreed at the beginning of the treatment are not being met, or if intolerable adverse events happen. Treatment should also stop if the goals can be achieved through other non-opioid treatments, or if there are concerns about a patient becoming dependent.
Brona Fullen, EFIC President said: “As the leading pain science organisation in Europe, it is crucial that EFIC sets the agenda on issues such as opioids, where there are growing societal concerns. These recommendations clarify what role opioids should play in chronic pain management, but also what role multimodal treatment plays.”
The paper’s lead author, Professor Winfried Häuser, commented: “The debate on opioid-prescribing for chronic non-cancer pain has become polarized: opioids are either seen as a dangerous risk for all patients, leading to addiction and deaths or they are promoted as most potent pain killers for any type of pain. This paper seeks to navigate the scientific and clinical evidence and provides recommendations for when opioids could be beneficial and when not for chronic non-cancer pain. Opioids are still important in the management of chronic non-cancer pain – but only in some selected chronic pain syndromes and only if established non-pharmacological and non-opioids analgesics have failed or are not tolerated.”
Immediate Past President and a co-author of the paper, Professor Bart Morlion said: “We have now reached a new European scientific consensus on opioid use for chronic non-cancer pain, which recommends that opioids should not be prescribed for many chronic pain conditions and serve only as a second- or third-line treatment in all others.”
-ENDS-
NOTES FOR EDITORS:
- The European Pain Federation (EFIC) is a multidisciplinary professional organisation in the field of pain research and medicine. Established in 1993, EFIC constituent chapters represent Pain Societies from 37 European countries and close to 20,000 physicians, basic researchers, nurses, physiotherapists, psychologists and other healthcare professionals across Europe, who are involved in pain management and pain research. For more information about EFIC, contact Sam Kynman, Executive Director, at sam.kynman@efic.org.
- The new clinical recommendations for opioid use in treating CNCP have been endorsed by:
- European Pain Federation (EFIC)
- European Academy of Neurology (EAN)
- European Federation of Addiction Societies (EUFAS)
- European Federation of Psychologists’ Associations (EFPA)
- European Psychiatric Association (EPA)
- European Region – World Confederation of Physical Therapy (ER-WCPT)
- European Society of Anaesthesiology and Intensive Care (ESAIC)
- European Society of Physical and Rehabilitation Medicine (ESPRM)
- European Society of Regional Anaesthesia & Pain Therapy (ESRA)
- Pain Alliance Europe (PAE)
- For additional mediamaterials, including videos, photos, author biographies and and opioid treatment infographic, visit the press area of our website at https://europeanpainfederation.eu/press-area/
- For media enquiries, contact our media liaison, Dennis Landsbert-Noon, at dln@panda-communications.com
Infographic
This version was published on March 11th 2021 and replaces all older versions.
Papers in full
Quotes
Winfried Häuser, lead author: “The debate on opioid-prescribing for chronic non-cancer pain has become polarized: opioids are either seen as a dangerous risk for all patients, leading to addiction and deaths or they are promoted as most potent pain killers for any type of pain. This paper seeks to navigate the scientific and clinical evidence and provides recommendations for when opioids could be beneficial and when not for chronic non-cancer pain. Opioids are still important in the management of chronic non-cancer pain – but only in some selected chronic pain syndromes and only if established non-pharmacological and non-opioids analgesics have failed or are not tolerated.”
Brona Fullen, President, European Pain Federation: “As EFIC President, I am delighted to present these new clinical practice recommendations that have been developed and endorsed by nine leading scientific societies and Europe’s leading pain patients‘ organization. From my perspective as a chartered physiotherapist, I also want to highlight the paper’s call for optimising access to non-opioid treatments that can include non-opioid medications, but also non-drug options such as exercise, physiotherapy or talking therapies for patients in need. These are treatments that EFIC has always advocated as being vital to treat pain effectively.”
Bart Morlion, Immediate Past President, European Pain Federation: “The situation surrounding opioids – and knowledge about how effective they are for different conditions – has been changing fast, which is why EFIC felt it was important to publish an update to our 2017 position paper on the use of opioids for pain management. We have now reached a new European scientific consensus on opioid use for chronic non-cancer pain, which recommends that opioids should not be prescribed for many chronic pain conditions, and serve only as a second or third line treatment in all others.”
Joop van Griensven, President, Pain Alliance Europe: “Pain Alliance Europe welcomes the new recommendations on opioid use for CNCP. This ensures and prioritises the communication between health care professionals and patients as the basis for the best possible (multi-disciplinary) therapy. This is a development that PAE has been advocating for years.”
Kevin Vowles, co-author: “Chronic pain is, by its very nature, a complex and multifaceted experience that affects almost every area of one’s life. The treatment of chronic pain by opioids is equally complex, as opioids have the potential for both benefit and harm, especially when taken over the longer term. The development of European guidelines was thorough and careful. Multiple disciplines were included in their development as this is the appropriate way to address the complexity of pain and opioids. Furthermore, there was an extensive external review and consultation process, when led to refinement of recommendations. Overall, these guidelines represent a consensus statement across a diverse range of clinicians and scientists that care for those with chronic pain.”
Videos
Interview with authors Bart Morlion and Kevin Vowles by Mary O’Keeffe, EFIC Fellow
Video statement from Winfried Häuser, lead author
Video statement from Brona Fullen, President, European Pain Federation EFIC
Video statement from Bart Morlion, Immediate Past President, European Pain Federation EFIC
Video statement from Joop van Griensven, President, Pain Alliance Europe