What is the biopsychosocial model of pain?
This model argues that pain is a personal experience that emerges from a dynamic interplay between biological, psychological, and social factors. These factors are not mutually exclusive. The European Pain Federation EFIC recommends comprehensive application of the biopsychosocial model of pain in clinical care (assessment and management), research, education (including EFIC’s Medicine, Physiotherapy, Nursing and Psychology Core Curricula) and policy.
The biopsychosocial nature of pain is promoted in the 11th revision of the International Classification of Diseases (ICD-11) and applies to all pain-related conditions. Particularly through the inclusion of the diagnosis of Chronic Primary Pain, which is defined as pain in one or more body systems, and in any body site, or in a combination of body sites that: (a) persists or recurs for longer than 3 months, (b) is associated with significant emotional distress (eg, anger, anxiety, or depressed mood) and/or significant functional disability (impacts on one’s activities of daily life, hobbies, and participation in social roles), and (c) includes symptoms that are not better accounted for by another diagnosis.
By acknowledging the role of emotional distress and function in the definition of chronic primary pain, the ICD-11 recognises that various factors affect pain – and so a promote a biopsychosocial model of assessment.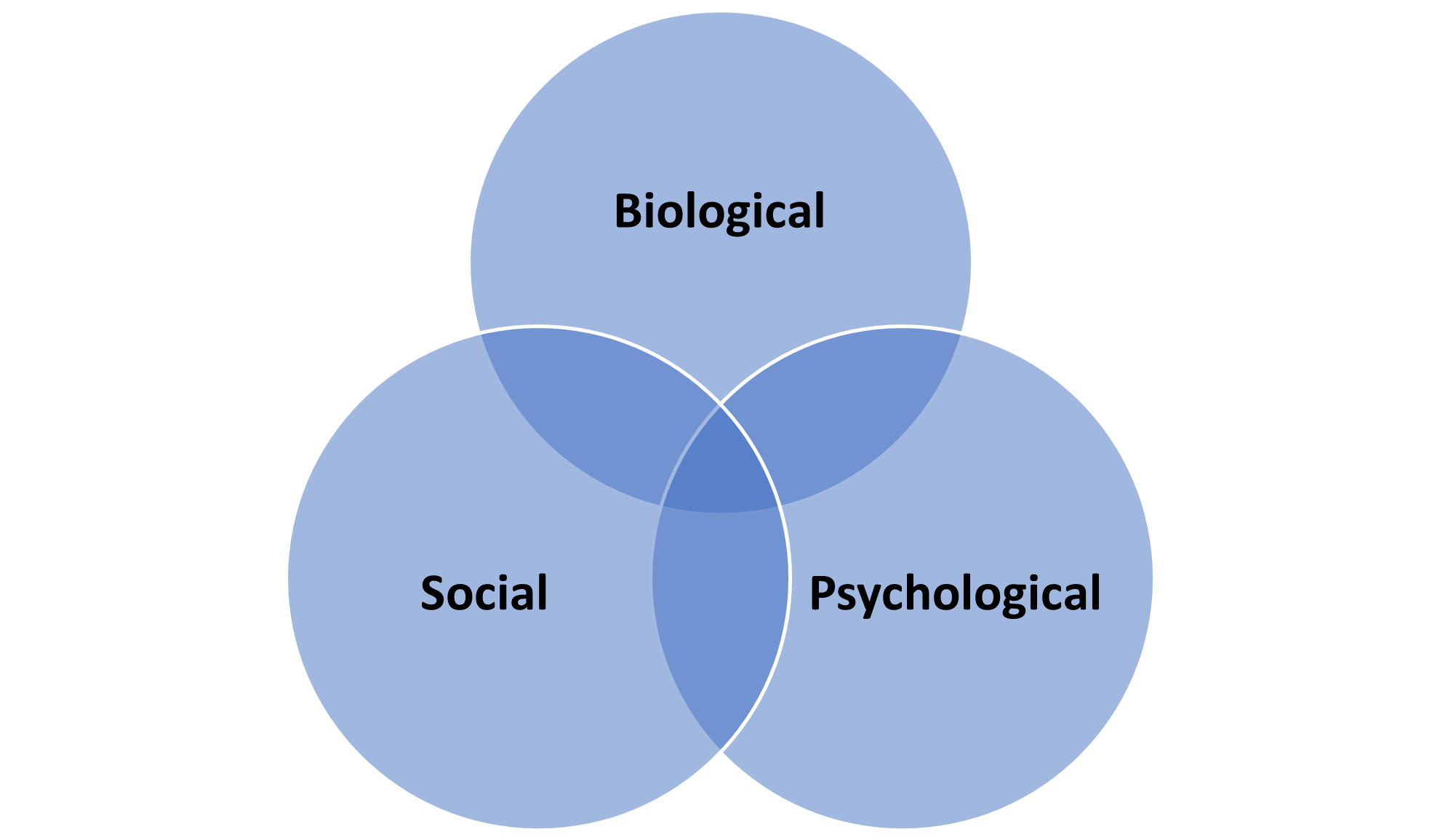
What does the bio (biological) in the model refer to?
Biological or physical factors can refer to genetics, magnitude of nociception, tissue injury, damage or disease, physical health problems, immune function, neurobiology and neurochemistry, effects of medications, sex differences, nervous system characteristics (e.g. pain threshold, pain tolerance, predisposition to peripheral, and central sensitisation), hormones, effects of lifestyle factors (e.g., sleep, weight, physical activity, alcohol, smoking), age, and endogenous pain modulation systems. It can also be used to refer to biomechanics and physical fitness (endurance, strength, flexibility).
What does the psych (psychological) in the model refer to?
Psychological factors refer to cognitions and emotions including mood, depression, anxiety, distress, anger, perceived injustice, coping styles (e.g. avoidance, endurance), fear, self-efficacy, catastrophising, personality, beliefs about causes and consequences of pain, attitudes, acceptance, and expectancies (e.g. about recovery).
What does the social in the model refer to?
Social or sociocultural factors refer to social expectations, social support systems (financial, instrumental, and emotional support), educational status, living status, work factors, finance or welfare issues, social deprivation or poverty, social disadvantage, exclusion, past pain experiences, health insurance, disability compensation, substance abuse, language and cultural barriers, exclusion, stigma, discrimination, and cultural factors.
Are multiple disciplines required to deliver a biopsychosocial approach?
No, not necessarily. A single discipline can use more than one approach to target biological, psychological, and social factors in a patient with pain. Treatments like pharmacotherapy, interventional pain management, surgery, manual therapy are often considered to target biological factors. Treatments like psychological approaches and patient education are considered to focus on psychological factors, while work or social support interventions may be considered to focus mainly on addressing social factors. Exercise may be delivered to target biopsychosocial factors depending on the treatment goals. If a single clinician combines evidence-based pharmacotherapy, embedded in education and a psychological approach, and a social support intervention, this could be considered a biopsychosocial approach.
However, a multidisciplinary or interdisciplinary approach (involving several disciplines) may be required for certain patients, both in terms of pain treatment and pain assessment. What constitutes a biopsychosocial approach (the number of disciplines and number of treatments required) can vary across countries, pain conditions, and pain duration, availability of services that can utilise an interdisciplinary approach (e.g. physicians, physiotherapists, psychologists, nurses, social workers working together as a team) to formulate an appropriate diagnosis and management plan.
Where can I find more about the biopsychosocial model of pain?
- EFIC resources:
-
Scientific resources:
- Raja, S.N., Carr, D.B., Cohen, M., Finnerup, N.B., Flor, H., Gibson, S., Keefe, F., Mogil, J.S., Ringkamp, M., Sluka, K.A. and Song, X.J., 2020. The revised IASP definition of pain: Concepts, challenges, and compromises. Pain, 161(9), p.1976.
- Nicholas, M., Vlaeyen, J.W., Rief, W., Barke, A., Aziz, Q., Benoliel, R., Cohen, M., Evers, S., Giamberardino, M.A., Goebel, A. and Korwisi, B., 2019. The IASP classification of chronic pain for ICD-11: chronic primary pain. Pain, 160(1), pp.28-37.
- https://www.iasp-pain.org/publications/relief-news/article/mechanistic-pain-management-biopsychosocial-model/
- Gatchel, R.J., Peng, Y.B., Peters, M.L., Fuchs, P.N. and Turk, D.C., 2007. The biopsychosocial approach to chronic pain: scientific advances and future directions. Psychological bulletin, 133(4), p.581.
- Turk, D.C. and Monarch, E.S., 1996. Biopsychosocial perspective on chronic pain. Psychological approaches to pain management: A practitioner’s handbook, 2.
- Nicholas MK. The biopsychosocial model of pain 40 years on: time for a reappraisal? Pain. 2022 Nov 1;163(Suppl 1):S3-S14.