What is the definition of pain?
Pain is an unpleasant sensory and emotional experience associated with, or resembling that associated with, actual or potential tissue damage. Pain is always a personal experience that is influenced to varying degrees by biological, psychological and social factors.
Nociception refers to the nervous system’s encoding of potentially damaging events (e.g. touching a hot stove, accidentally cutting yourself). But one can experience pain without nociception and have nociception without pain. Pain does not equal nociception. Nociception is objective, but pain is subjective and does not emerge solely from activity in sensory neurons.
Through their life experiences, individuals learn the concept of pain. A person’s report of an experience as pain should be respected.
Although pain usually serves an adaptive role, it may have adverse effects on function and on social and psychological well-being. Verbal description is only one of several behaviours to express pain, as the inability to communicate does not negate the possibility that a human or a nonhuman animal experiences pain.
Acute pain versus chronic pain
Pain that resolves reasonably quickly is referred to acute pain. Pain that lasts a long time is called chronic or persistent pain.
Definitions of acute and chronic pain can vary.
Some state that acute pain lasts less than 30 days, while others state that acute pain can refer to any pain that resolves before 3 or 6 months. Acute pain is seen as a useful survival mechanism that serves a protective and healing function.
Chronic pain is most often defined as pain lasting longer than 3 to 6 months. The IASP Classification of Chronic Pain for the International Classification of Diseases (ICD-11) is defined as pain that persists or recurs for more than 3 months. The pain can be the main or sole clinical problem in some patients. ((Reference: Treede RD, Rief W, et al. Chronic pain as a symptom or a disease: the IASP Classification of Chronic Pain for the International Classification of Diseases (ICD-11). Pain. 2019 Jan;160(1):19-27. doi: 10.1097/j.pain.0000000000001384.)
Chronic pain is a complex phenomenon involving a dynamic interaction between various biological, psychological and social factors.
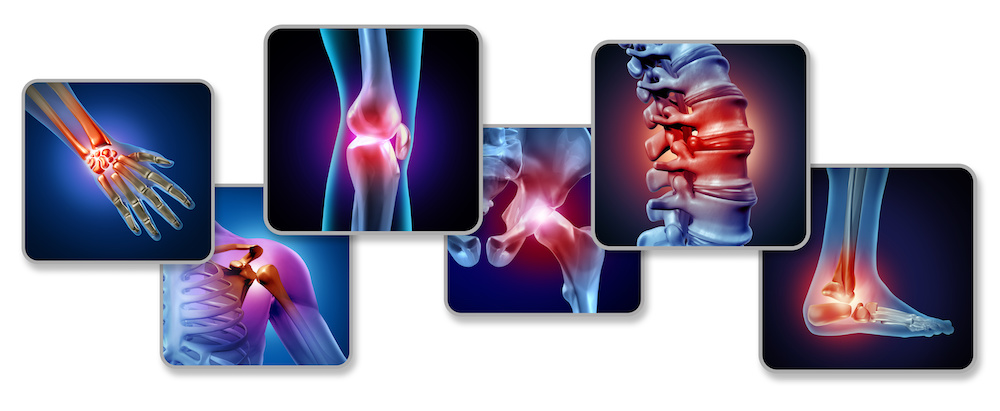
What are the most common pain syndromes?
The answer to this question may vary across countries and specific subgroups (e.g. older vs younger adults) but spinal pain (particularly low back pain), headaches, osteoarthritis pain, fibromyalgia (widespread pain), cancer pain, post-surgical pain and neuropathic pain are common and responsible for high levels of disabilities worldwide.
Is chronic pain a symptom or a disease?
This is currently a heavily debated area.
Traditionally, chronic pain would have been viewed as a symptom and would not have been represented in a systematic manner in the World Health Organisation (WHO) International Classification of Diseases (ICD). Some feel this has hampered attempts to better define and treat pain as it hasn’t been adequately recognised compared to other health conditions.
Some are now proposing that chronic pain should be conceived as a disease in its own right, and be referred to as ‘chronic primary pain’, and indeed this is the case with the latest update to the ICD. This would include common syndromes like low back pain not caused by a serious pathology (e.g. cancer, a broken bone) and fibromyalgia.
Where pain may at least be initially conceived as a symptom only, there are now calls to refer to these instances as chronic secondary pain. This refers to chronic cancer-related pain, chronic neuropathic pain, chronic secondary visceral pain, chronic posttraumatic and postsurgical pain, chronic secondary headache and orofacial pain and chronic secondary musculoskeletal pain.
How many people are affected by chronic pain?
It is difficult to state an exact number, but the burden of pain conditions is substantially high.
The Global Burden of Disease Study 2016 found pain and pain-related diseases, particularly low back pain and migraine, are the leading causes of disability and disease burden globally. Low back pain and migraine are responsible for 57.6 million and 45.1 million years of life lost due to disability, respectively. This means the burden of pain conditions is higher than that due to depression, cancers, diabetes and Alzheimer’s disease.
In Europe alone, almost one in five individuals or 20% of the adult population report having moderate or severe chronic pain. This means there are 150 million people in Europe experiencing chronic pain.
Chronic pain has been linked to numerous physical and mental conditions and contributes to high health care costs, early retirement and productivity lost.
In 2004, in response to chronic pain being a widespread public health problem, the International Pain Society and Global Health Community stated that “failure to treat pain is viewed worldwide as poor medicine, unethical practice, and an abrogation of a fundamental human right.”

How is pain currently managed in Europe?
Pain management in Europe centres around a biopsychosocial approach. The model refers to the development of pain through the complex interaction of biological (genetic, biochemical, etc.), psychological (mood, thoughts, beliefs) and social (cultural, familial, socioeconomic, etc.) factors.
As such, pain management consist of pharmacological approaches (e.g. medicines), non-pharmacological approaches (e.g. exercise, cognitive behavioural therapy), patient education, invasive approaches where needed, and long-term pain management programmes for people with persistent/chronic pain.
Can we measure pain?
Yes. Measures are self-reported. There are no currently no valid objective measures – e.g. a blood test or scan for detecting pain. The only way of knowing if a person has pain is if they tell you – as pain is a subjective and personal experience.
A number of questionnaires are used to measure the intensity of a person’s pain or the disability related to the pain. The most popular measures are numerical and visual analogue scales where patients will be asked to rate their pain on a scale of 0-10 or 0-100.
Some measures are specific to a person’s pain syndrome – e.g. low back pain disability measures and headaches disability measures.
Measuring pain in children or specific subgroups like dementia can be a bit more difficult and relies on behavioural observations.
Downloads
Feel free to download these visuals and infographics which are a great resource for clinicians who want to give their patients some basic introductory information on pain.