What is Chronic Primary Pain?
Chronic primary pain (CPP) is term that has been implemented in the latest revision of the International Classification of Diseases (ICD-11), which came into effect in 2022. It is defined as pain in one or more body systems (eg, nervous, musculoskeletal, and gastrointestinal systems), and in any body site (face, low-back, neck, upper-limb, thorax, abdominal, pelvis, and urogenital region), or in a combination of body sites (eg, widespread pain) that:
(1) persists or recurs for longer than 3 months
(2) is associated with significant emotional distress (eg, anger, anxiety, or depressed mood) and/or significant functional disability (impacts on one’s activities of daily life, hobbies, and participation in social roles),
(3) and the symptoms are not better accounted for by another diagnosis.
Therefore, the chronic pain is the dominant clinical problem and is considered a condition in its own right. Before a diagnosis of chronic primary pain can be made, diagnoses that could explain this pain need be ruled out through a proper assessment. If the pain can be accounted for by another diagnosis, it will be categorised as a form of chronic secondary pain which includes chronic cancer pain, chronic postsurgical or posttraumatic pain, chronic neuropathic pain, chronic secondary headache or orofacial pain, chronic secondary visceral pain, and chronic secondary musculoskeletal pain.
What clinical presentations are categorized as chronic primary pain?
Many chronic pain conditions have unclear causes and pathophysiology. They are better represented by a complex interaction between biological, psychological, and social factors that vary from individual to individual. The following pains are considered chronic primary pain:
- Chronic widespread pain (CWP) such fibromyalgia
- Complex regional pain syndrome
- Chronic headaches and orofacial pain: migraine, tension-type headache, trigeminal autonomic cephalgias, temporomandibular disorders, burning mouth, orofacial pain
- Chronic visceral pain: chest pain syndrome, epigastric pain syndrome, irritable bowel syndrome, abdominal pain syndrome, bladder pain syndrome, pelvic pain syndrome
- Chronic musculoskeletal pain (other than orofacial): cervical pain, thoracic pain, low back pain, limb pain
Chronic widespread pain
Chronic widespread pain (CWP) is musculoskeletal pain which presents diffusely in at least 4 of the 5 body regions and in at least 3 body quadrants (upper-lower-left-right of the body) and axial skeleton (neck, back, chest, and abdomen) [1]. There are several core attributes of CWP, including pain persisting for at least three months alongside signs of significant emotional distress or functional disability. This category includes fibromyalgia as a form of CWP. Diagnosis for this condition can be difficult but may be indicated if the physiological cause of pain or nociceptive activity cannot be determined, and significant nociplastic (e.g. hyperalgesic), psychological or social contributors are present. Conditions, such as obesity and diabetes are often associated with CWP highlighting an increase in comorbidities in people presenting with this condition.
Complex regional pain syndrome
Complex regional pain syndrome (CRPS) is characterized by spontaneous regional pain, often beginning distally, that is disproportionate (in magnitude or duration) to the typical course of pain after similar tissue trauma [3]. The condition is identified by various signs of autonomic and inflammatory changes that can vary among patients and change over time. Symptoms such as hyperalgesia, skin colour and temperature changes, sweating, reduced strength, tremors and dystonia may be reported in the affected limb. Two subtypes of CRPS have been outlined; type 1 and type 2. Both can occur after trauma however, type 1 indicates there is no evidence of peripheral nerve injury, whilst type 2 requires this for diagnosis. Chronic pain after peripheral nerve injury is also considered an additional parent of the diagnosis.
Chronic primary headache or orofacial pain
Chronic primary headache or orofacial pain is defined as headaches or orofacial pains that occur for more than two hours per day on at least 50% of the days during the last 3 months [4]. Other diagnoses to be considered are listed under chronic secondary headache and orofacial pain. Diagnosis of chronic primary headache or orofacial pain is based on the current phenotype of the reported headache with each distinct type, subtype or sub form of headache being coded and diagnosed individually. In the case of a patient receiving multiple diagnoses, prioritisation should be based on the patient’s preference. Several sub types of chronic primary headache or orofacial pain can be defined: chronic migraine, chronic tension-type headaches, trigeminal autonomic cephalalgias, chronic temporomandibular disorder and chronic burning mouth pain. To find out more about sub-types of chronic primary headache, read Nicholas et al, 2019. [5].
Chronic primary visceral pain
Chronic pain localised to the head, neck, thoracic abdominal or pelvic region may be related to Chronic primary visceral pain. The respective location of pain may coincide with typical referral patterns from internal organs. Examples may be from the thoracic region (e.g. non-cardiac chest pain or reflux hypersensitivity), abdominal region arising from the viscera of the digestive system (e.g. IBS, epigastric pain syndrome) and in the pelvic region via the urinary, digestives and genital systems (e.g. bladder pain syndromes, chronic pelvic pain). Subtypes of chronic primary visceral pain should be considered [2]. Chronic primary chest pain, chronic epigastric pain syndrome, irritable bowel syndrome (IBS) and chronic primary abdominal, bladder and pelvic pain syndromes are included in the subtypes of primary visceral pain and can be explored further here.
Chronic primary musculoskeletal pain (other than orofacial)
Chronic primary musculoskeletal pain is located in muscles, bones and tendons. Some of the most common examples of this include cervical, thoracic, lumbar and limb pains. These syndromes are distinguished by location: chronic primary cervical/thoracic/low-back/limb pain respectively. Reported symptoms may include localised pain and allodynia and/or hyperalgesia presenting either spontaneously or upon being evoked [2].
How to diagnose chronic primary pain?
As mentioned previously, to diagnose chronic primary pain, ruling our other causes of the reported symptoms is required. Identification of factors which are contributing to the individual’s pain experience is required. This can be achieved by conducting a multifactorial, person-centred assessment exploring potential causes related to aspects of biological, psychological, and sociological constructs. This includes, but not limited to, an assessment of the patient’s clinical presentation using a structured and evidence-based guided assessment (including consideration of primary and secondary differential diagnoses) alongside assessment of the patient’s relevant medical history. An example can be found in EFIC clinical recommendations for the diagnosis and management of CRPS and further advice can be found here.
What is ICD-11?
ICD-11 is the World Health Organisation (WHO)’s global standard for diagnostic health information. To overcome the inadequate classification of chronic pain in ICD-10, IASP set up a Task Force with the aim of developing a systematic classification system for chronic pain. ICD-11 codes list is used to record individual health conditions and causes of death. These data can be utilized for a wide variety of purposes, including reimbursement, research, and policy planning. To visit ICD-11 online or ICD-11 download, please visit https://icd.who.int/browse11/l-m/en.
ICD 11 vs ICD 10
Chronic pain was not represented adequately in ICD-10. The complex biological, psychosocial, and social aspects of pain were not acknowledged. Pain was often sub-grouped according to physical or psychological causes, disregarding the social component of the pain experience. Given recent advances of research related to the influence of social factors within the chronic pain experience, the ICD-10 classifications are not well represented and provide little diagnostic value for chronic conditions. For pain with which a clear pathophysiological aetiology was not present, and when a combination of biological, psychological and social factors were indicated, the only classification available according to the ICD-10 was ‘somatoform pain presentation’ [2]. New classifications featured in the ICD-11 may provide more consistent subgrouping of categories related to diagnoses, especially when it comes to delivering multimodal pain management. Codes related to multiple chronic conditions may have previously been invisible to the ICD-10 (such as chronic cancer pain, chronic neuropathic pain, chronic musculoskeletal pain and chronic postsurgical pain) and are now able to be coded in a precise and meaningful manner using the ICD-11. A direct comparison of codes within the ICD-10 and ICD-11 shows that the information contained within the ICD-11 codes are more useful for clinical management, monitoring, research and teaching [6]. This suggests that individual diagnoses within the ICD-10 were poorly defined and may have been scattered through the coding list. Not only is the coding system within the database more expansive, the ICD-11 has become more ‘user-friendly’. Embedded within its ‘digital health ready’ approach, is the increased ease of use and accuracy of coding of which now requires less user training than the previous version, alongside online and offline functionality.
You can access an ICD-11 fact sheet here.
Why do we need ICD-11?
The lack of standardization in recording and reporting pain diagnoses not only has negative impacts on individuals’ treatments, social activities, and overall quality of life, but also on patient organization’s abilities to understand global health states. Effective systematic classification may improve research strategy, via increased accuracy of epidemiological data at global level influencing not only health services but also policy makers. Implications to the development of policy is of huge significance, specifically in that the ICD-11 will increase the recognition of chronic pain as a health problem and contribute to better access of treatments. The ICD-11 integrates the coding process into electronic health records allowing increased efficiency in data processing and supporting multimodal care. Utilising the advancements of the ICD-11, which recognizes chronic pain with systematic classifications, will contribute to the consistency of chronic pain diagnosis thus improving patient treatment, alongside the quality of both scientific research and policy initiatives for the management of chronic pain. Read more about EFIC’s ‘letter to the editor’ exploring why we need to implement the ICD-11.
How can I adequately code pain using ICD-11?
Using the online tool available here, searching for ‘Chronic Primary Pain’ will reveal several options. Exploring the postcoordination, by clicking on the ‘+’ icon to the left, will expand the selection to reveal all potential codes for that category.
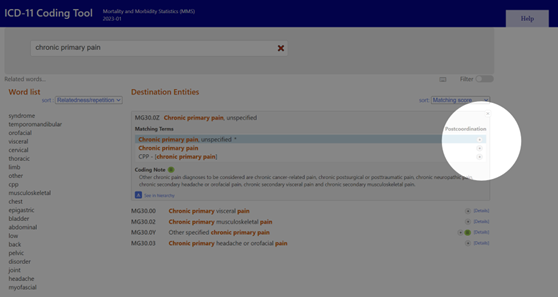
Image: indication of option to view additional codes within selection.
From here, you will be presented with the complete library of the ICD-11. Navigating the left panel, which includes information on the sub-types of CPP, and selecting the appropriate option will display the postcoordination information for that diagnosis. Here, you can then choose codes by clicking on the appropriate options. You can see from the image below that individual options are coded. For example, chronic widespread pain for which psychosocial factors are present, alongside moderate pain, distress and pain-related interference of an intermittent nature would be coded as “MG30.01&XS7G&XS9Q&XS7C&XS2L&XT5G”.
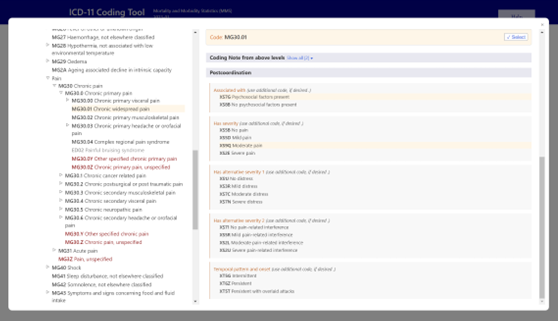
Image: display of codes available for Chronic widespread pain within the ICD-11.
This process can be repeated for all manner of conditions within the database. Other options of diagnosis, for example complex regional pain syndrome, will include additional coding options relating to the laterality and the anatomical location of the symptoms. Additional ICD-11 tutorials and instructional materials, which are provided by the WHO, cover topics such as; ‘An introduction to ICD-11’, using the ICD-11 coding tool and gaining access to the ICD-11 coding list, and Death Certification and can be found here.
Treatment approaches for chronic primary pain
Treating chronic pain can be difficult, not just for patients but also for clinicians. Unfortunately, there is no ’gold standard’ however, there are a few things you should consider when thinking about managing chronic pain. Utilising a holistic approach within a biopsychosocial framework that can be accesses not only in the primary care setting, but also in secondary and tertiary care which provides strong emphasis on the delivery of multidisciplinary evidence based practice is suitable. To achieve this, a range of interventions can be considered:
Pharmacotherapy: The World Health Organisation provide information relating to the pharmacological management of chronic primary pain [7]. You can explore their recommendations here.
Physical activity & exercise: As far as evidence goes, promoting physical activity is something that can help a patient’s pain in the long-term. Patients and clinicians should seek to develop progressive and sustained levels of physical activity as part of an individualised multimodal pain treatment plan. The physical activity components of treatments for chronic pain should focus on not only the biomedical aspects, but also the psychological and social benefits of exercise whilst addressing barriers to long-term adherence. Ensuring effective behaviour change throughout the processes of treatment, via engagement of support networks, utilisation of social networks may facilitate adherence. Exercise programs should aim to improve mental health, physical fitness and everyday quality of life [8]. For more information, visit the On The Move Campaign.
Psychological strategies: Cognitive behavioural therapies (CBT) or acceptance and commitment therapies (ACT) may improve quality of life for people with chronic primary pain. There is limited evidence of some benefit for relaxation, mindfulness, psychotherapies and hypnosis for the management of chronic primary pain. It may be suitable to consider these approaches, however, ensuring CBT or ACT interventions are delivered by healthcare professionals with appropriate training is key [7]. It may also be useful to assess the significance of providing additional interventions to address behaviour change and educational strategies promoting disease knowledge, self-management and more broad aspects of health literacy such as health-related communication (see EFIC Plain Talking Campaign).
Understanding your condition: Education should be part of good clinical practice and increasing an individual’s understanding of their condition is important to promote self management approaches. For this to happen effective communication through considering health literacy sensitive approaches need to be adopted.
References
EFIC Webinar on Chronic Primary Pain
Watch this recording from a webinar on 28 April 2023 where we aimed to give an overview on the definition and new classification under ICD-11 as well as more information on the assessment and management of chronic primary pain.