Integrated Pain Management
Initiate policies to integrate pain management as a core component of quality healthcare and a core part of patient care for many co-morbidities.
We ask policy makers to promote the systematic integration of multidisciplinary and multimodal pain management within healthcare systems. This includes promoting dedicated networks of pain clinics and multidisciplinary hospital pain services, as well as embedding pain management in services for which pain plays a major role as a comorbidity, such as cancer and mental health services.
We call on the European Commission to:
- Recognise the important role pain management plays within healthcare systems and the need for systematic inclusion of pain management considerations within European healthcare strategies.
- Support the development of pain management centres of excellence across Europe and encourage a network for these centres to spread expertise and promote best practices across Europe.
- Support the development of centres of excellence in pain management across Europe and foster a collaborative network to enhance understanding and to improve the quality and sustainability of services.
We call on national governments to:
- Establish dedicated pain management clinics and hospital pain services, incorporating evidence-based guidance and best practices on multidisciplinary and multimodal pain treatment.
- Identify a national pain services lead within the healthcare system, to coordinate the country’s approach to pain management and maintain standards.
- Ensure equitable access to pain services across all population groups, with attention to underserved communities such as deprived populations, rural areas, older adults, women, migrants, and LGBTQ+ communities.
Our commitments:
- To foster best practices and evidence-based guidance to support healthcare systems, and to set high standard for pain education across Europe to elevate the knowledge and competences of healthcare professionals available to national healthcare systems
Further Information
- SIP 2019: Joint Statement implementation – Pain education
- Interview with Dr. Emma Briggs SIP@EFIC
- Interview with Dr. Andreas Kopf SIP@EFIC
- Video Statement: Francoise Thomas – Pain Education
- Joint Declaration of SIP Portugal 2019: Employment and Education
- SIP 2017, Working Group 1: Andreas Kopf – Education: Do we still need it?
- National initiatives United Kingdom: Better education on pain management – press release
- SIP 2012, Working Group 4: Kris Vissers – Education and research Programmes on pain management in EU
- SIP 2012, Working Group 4: Begoña García Cepeda – Education in pain
- SIP 2012, Working Group 4: Manuela Monleón / Marta Pisano – Developing pain education for nurses by nurses
- SIP 2011, Workshop 2: Jan Dobrogowski – Can education in pain improve the treatment of pain?
Previous Strategic Focus Areas
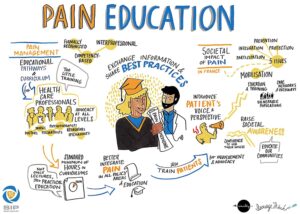
Pain Education
Pain medicine is not taught as a dedicated unit in most European medical schools and there is a lack of awareness of the societal impact of pain in the broader community.
- Formal academic pain education
Pain education within the medical curricula remains limited. In a study published in 2015[1], it found that even if pain was taught, it was not within a specific pain module.
At EU level, the Joint Action on Health Workforce Planning and Forecasting (EU JAHWF)[2] launched a three-year project to map existing activities and to create a list of good practice examples. In 2016, it published a handbook on “health workforce planning methodologies that describes and analyses the planning practices developed in selected EU countries”[3]. The outcome of the Joint Action was the establishment of the health workforce planning and forecasting expert network, which aims to create a platform for exchanging knowledge and best practice. It also aims to address challenges across the EU.
- Awareness raising and wider stakeholder education
Alongside formal academic education, education of other stakeholders is of equal importance. Notable stakeholders include policymakers, patients, healthcare management, and employers/employment organisations and unions. Such education should, furthermore, be tailored to the specific audiences, their level of health and pain literacy, and take into account their respective cultural and social backgrounds.
There has been limited EU- or Member State-led activity in relation to specific pain-focused awareness raising activities. Most awareness raising activities have been conducted by civil society, aimed at the general public as well as to policymakers.
At EU level, the European Commission funded the EMPATHiE (Empowering patients in the management of chronic diseases)[4] study in 2014, which sought to contribute to EU knowledge and facilitate the development of patient-centred healthcare policies, whilst also contributing to the then-reflection process on chronic disease management. The study looked at four different working packages: 1. Identification of best practice models for patient empowerment, 2. Analysis of these models and identification of advantages and barriers to empowering patients, 3. Develop a methodology to validate the transferability of good practice, and 4. Develop scenarios for future EU collaboration regarding patient empowerment.
On the other hand, a number of civil society-led awareness raising platforms exist. Those aimed at policymakers include the SIP Platform Annual Symposium and the European Parliament Brain, Mind, and Pain (BMP) Interest Group[5]. Activities aimed at the wider general public include International Pain Awareness Month[6] and the Pain Toolkit[7].
SIP Recommendation for Policy Action
Prioritise pain education for health care professionals, patients, policymakers, and the general public
SIP calls on the European Commission and Member States to facilitate the sharing of best practice and identification of gaps.
SIP also calls on the European Commission and Member States to propose recommendations to educate healthcare professionals, patients, policymakers and the general public on the issue of pain and its impact across Europe.