Access to Treatment
What is Pain?
Pain is the one of the most prevalent medical conditions in Europe and worldwide. It is the most common reason people seek health care and is the number-one cause of disability and reduced quality of life. There is a strong socio-economic gradient in terms of prevalence and impact, particularly for work disability and sickness absence. Disability burden due to pain is escalating, threatening the sustainability of European healthcare and social systems. However, pain research is significantly underfunded compared to other areas of health research and this underinvestment is considered a key factor contributing to the burden. The European Commission has called many pain conditions high-burden and under-researched, requiring substantial attention.
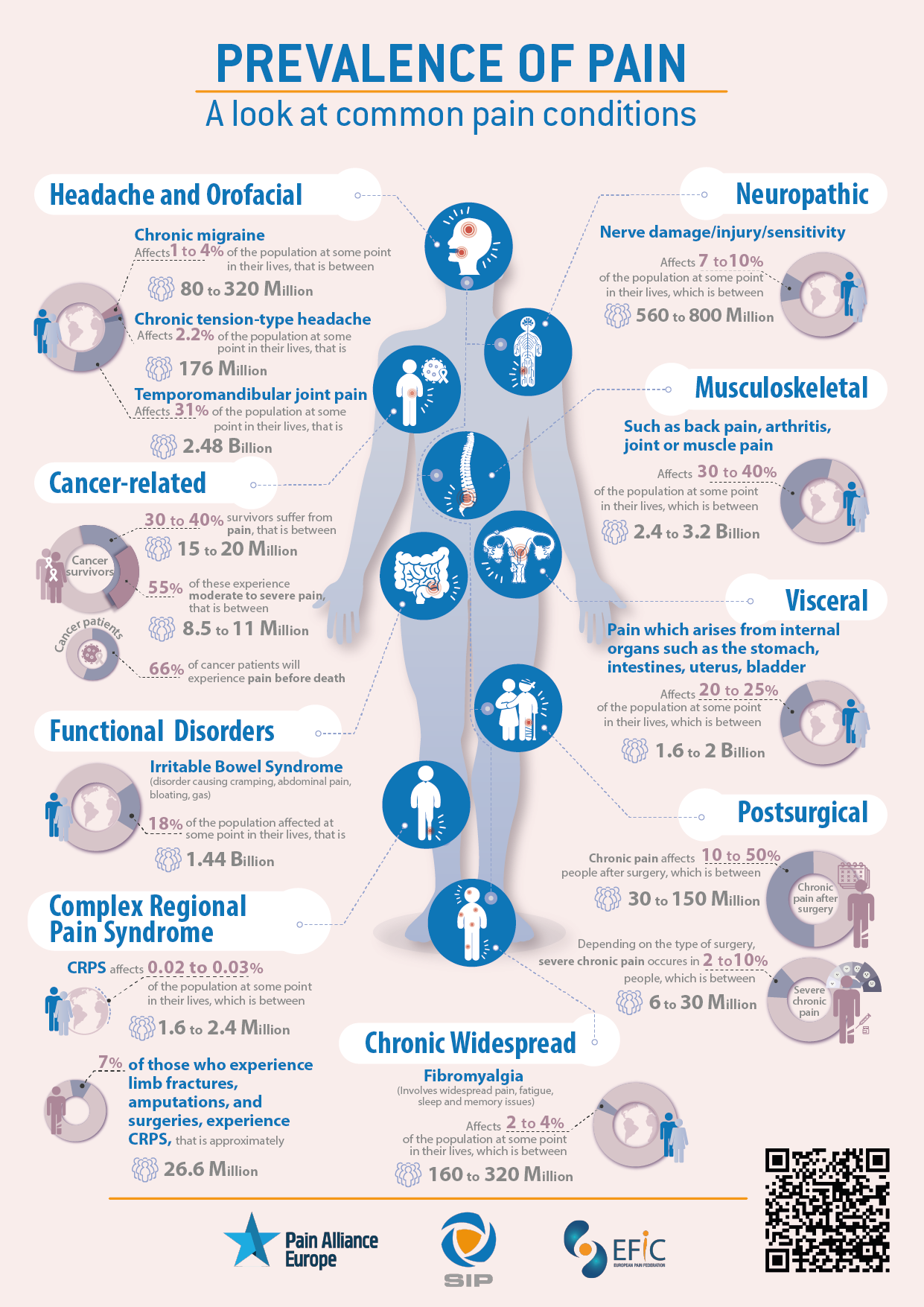
According to the Global Burden of Diseases, Injuries, and Risk Factors Study 2020, which includes a comprehensive assessment of incidence, prevalence, and years lived with disability (YLDs) for 354 causes in 195 countries and territories from 1990 to 2017, pain related conditions such as headache disorders (e.g. migraine) and musculoskeletal pain disorders (e.g. low back pain, hip and knee osteoarthritis, neck pain) are two of the largest contributor to years lived with disability (YLDs). Back pain and migraine are responsible for 57.6 million and 45.1 million years of life lost, due to disability, respectively.
In Europe there are approximately 740 million people, most of whom experience an episode of severe pain at some point in their life. For approximately 20 percent, that pain persists for longer than three months and these have chronic pain. Therefore, at present, 150 million people are experiencing chronic pain across Europe, this is approximately equal to the population of Germany and France combined.
Statistics do not truly show the impact pain has on the individual or their loved ones. Pain has a devastating impact on those who are suffering. It can take hold of one’s life, destroying one’s ability to engage in hobbies, walk short distances, work, or go out with friends (e.g., going out to the cinema because it is too painful to sit for a long time). Pain oftens wakes people up and ruins the ability to sleep. Constant feelings of excessive tiredness, in addition to pain, mean people struggle to concentrate and manage everyday tasks. The pain often becomes the dominating factor in the sufferer’s life. It contributes to diminished well-being, limitations in mobility and social marginalisation across their lifespan, and it is associated with depression, cancer and cardiovascular-related mortality, as well as with a lower life expectancy. Loved ones are also negatively affected in numerous ways such as emotional stress (e.g. feeling helpless when they see someone they care about in pain), changes in relationship dynamics (e.g. reduced quality time due to the person being limited in what they can do), financial problems (the cost of tests and treatments for the person with pain), and increased caregiving responsibilities (helping a person manage their pain can be physically and emotionally demanding) leading to burnout and exhaustion over time.
Large proportions of individuals in Europe with chronic pain have inadequate pain control with previous estimations being as high as 40%. There are substantial gaps in our understanding of the causes and consequences of many pain conditions, and a noticeable lack of research persists across many European countries. This scarcity of data makes it challenging to generalise research findings to all EU member states. The uptake of the Recommendations presented at the end of this document, is critical to advancing the knowledge on the societal impact of pain.
The Burden of Pain
The Societal Impact of Pain (SIP) Platform has developed a Book of Evidence entitled ‘The Burden of Pain: A Societal Impact of Pain (SIP) Book of Evidence‘, targeted at individuals from a non-scientific background (e.g. policymakers and funding organisations) to gain an insight into what pain is, understand different definitions used (e.g. acute pain, neuropathic pain, nociceptive pain), and the debilitating effects pain has on patients and societies.
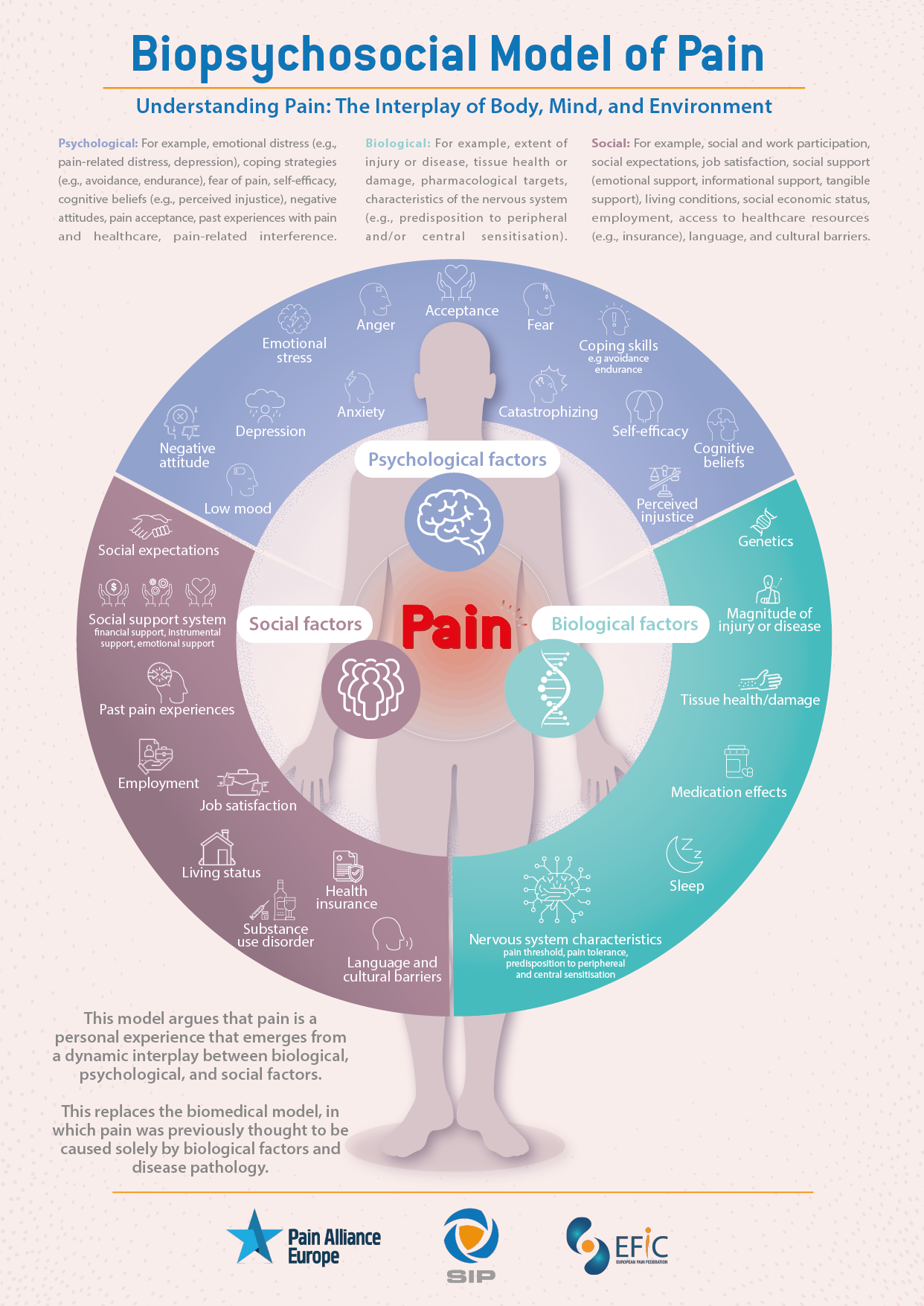
The document explains distinct types of pain conditions (e.g. headaches, low back pain), how common they are, treatment approaches, and common co-occuring health problems, as well as crucial concepts and challenges in the pain field, including pain measurement and assessment, chronic pain stigma, the importance of acknowledging the personal multidimensional nature of pain that requires an appreciation of the interplay between myriad biological/physical, psychological, and sociocultural factors.
Overall, the document describes what pain is and draws attention to the need for urgent policy action and increased funding for research. In particular, the Recommendations highlighted at the end of the document are a call to action to the European Commission, European Parliament, European Council and civil society to address the disastrous societal impacts of pain.
The Societal Impact of Pain (SIP) Platform will continue to raise awareness about the devastating impact pain has on sufferers, societies and economic systems; exchange information and best practices across all members states of the European Union; and develop and foster European-wide policy strategies and activities for an improved pain care paradigm in Europe.
The Burden of Pain: A Societal Impact of Pain (SIP) Book of Evidence
The Societal Impact of Pain (SIP) Platform, calls upon EU and national policymakers to:
- Recognise the burden and impact of pain on societies and patients, and increase its priority within healthcare systems, funding and policymaking.
- Ensure the effective implementation of ICD-11, as its use allows international agreement on the use of standardised diagnosis and tools and improves the recollection of data for both primary and secondary use.
- Ensure patient registries are established and frequently used, as it will improve the understanding of pain and pain management and treatment.
- Pain as a quality indicator: Develop instruments to assess the impact of pain.
- Pain research: Increase investment in research on better understanding the causes (pathophysiology) of various pain conditions, developing novel pain treatments, understanding and addressing comorbidity between pain and mental health conditions, increasing development and use of patient reported outcome measures for all pain conditions, establishing a gold standard for self-management programmes, and increasing access to high quality care.
- Pain in employment: Initiate policies addressing the impact of pain on employment and work productivity and include pain in relevant existing initiatives.
- Pain education: Prioritise pain education for healthcare professionals, patients, policy makers and the general public.
- Information technology for pain: Development of interoperable digital health ecosystems featuring accessible digital solutions for pain evaluation, monitoring and management (apps, online resources etc.) and legal and regulatory frameworks for data sharing.
Download the full Book of Evidence here.
Translations
- Please find the Dutch translation of the SIP Book of Evidence here.
- Please find the French translation of the SIP Book of Evidence here.
- Please find the German translation of the SIP Book of Evidence here.
- Please find the Portuguese translation of the SIP Book of Evidence here.
- Please find the Slovenian translation of the SIP Book of Evidence here.
- Please find the Spanish translation of the SIP Book of Evidence here.
- Please find the Swedish translation of the SIP Book of Evidence here.
- Please find the Maltese translation of the SIP Book of Evidence here.
- Please find the Finnish translation of the SIP Book of Evidence here.
Translations
- Please find the Danish translation of the Prevalence of Pain Infographic here
- Please find the Danish translation of the Biopsychosocial Model of Pain Infographic here
- Please find the Danish translation of the Common Pain Conditions Infographic here
- Please find the Danish translation of the Life with Chronic Pain Infographic here
- Please find the Spanish translation of the Prevalence of Pain Infographic here
- Please find the Spanish translation of the Biopsychosocial Model of Pain Infographic here
- Please find the Spanish translation of the Common Pain Conditions Infographic here
- Please find the Spanish translation of the Life with Chronic Pain Infographic here
Video Statements
Endorsers and Quotes
A High-Quality Policy Framework for the Delivery of Pain Care
The proposed policy framework for the delivery of pain care template aims to address the significant challenges faced by individuals living with pain in the respected country, and therefore serves as a comprehensive framework to improve pain treatment and management, enhance patient outcomes, and reduce the burden of pain.
A quality policy framework for the delivery of pain care encompasses several key elements aimed at effectively addressing the challenges associated with pain management, treatment and how national health systems should be organised. While the implementation of specific details is likely to vary depending on the individual country and healthcare system, there are some essential components that a comprehensive and high-quality policy framework for the delivery of pain care should include.
Please find the SIP Policy Framework for the Delivery of Pain Care document here.
Please find the leaflet summing up the main takeouts from the SIP Policy Framework for the Delivery of Pain Care here.